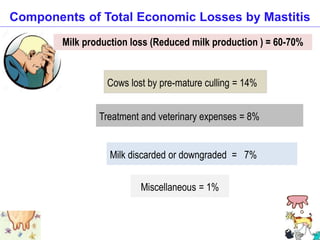
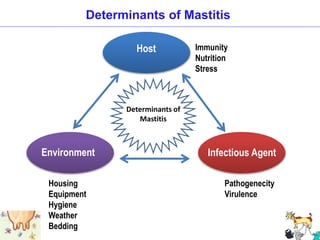
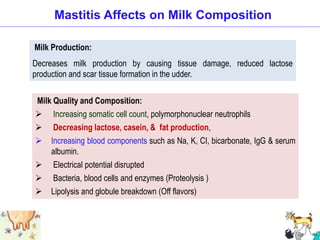
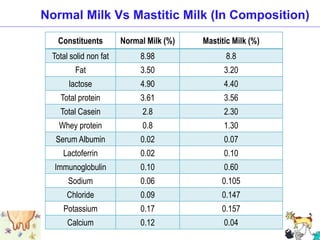
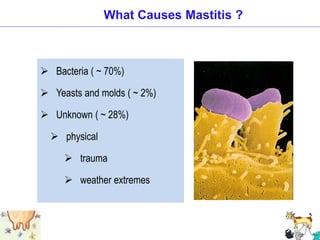
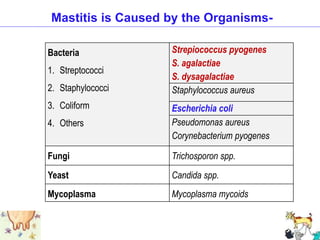
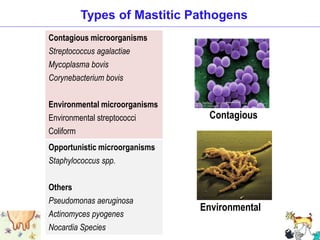
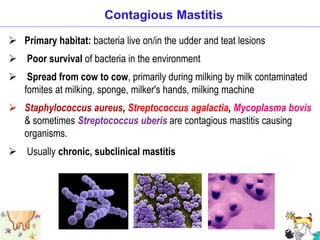
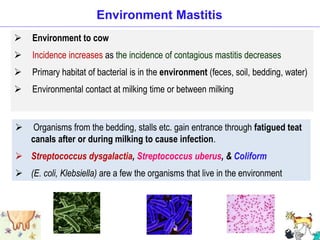
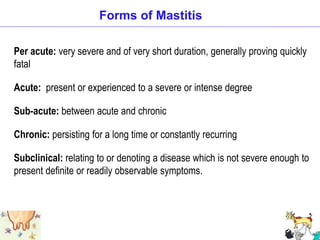
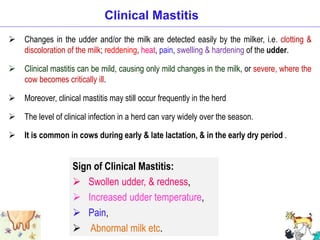
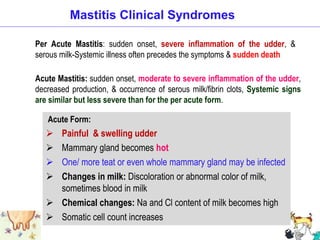
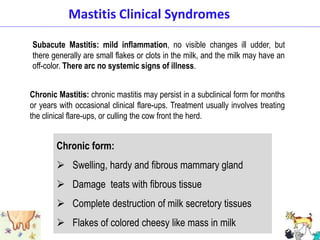
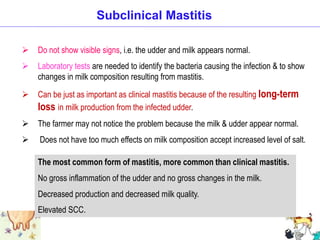
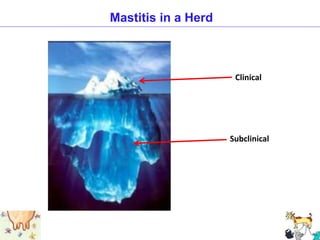
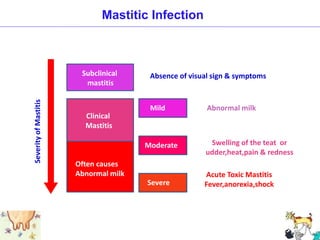
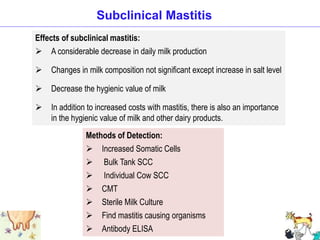
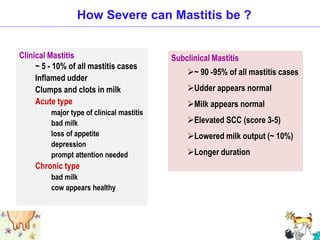
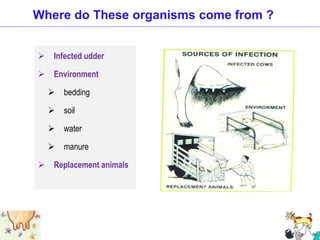
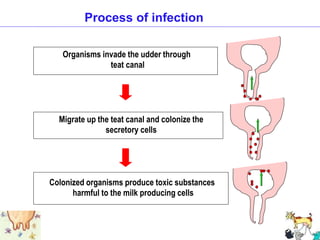
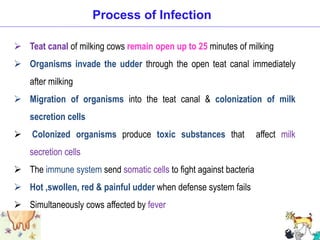
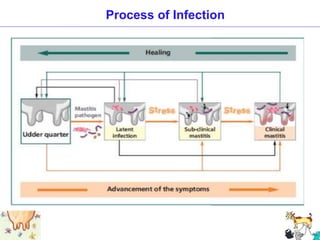
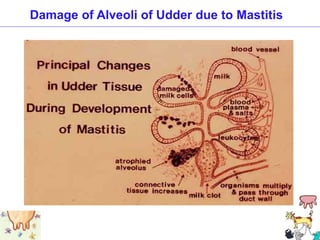
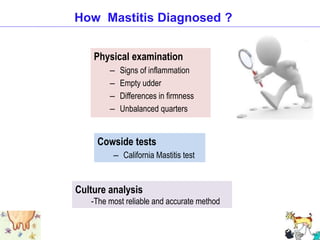
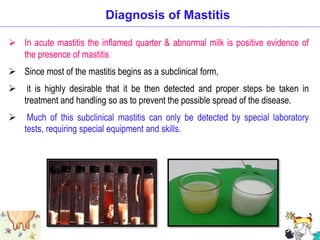
Mastitis is an inflammation of the mammary gland that can be clinical or subclinical. It is caused most commonly by bacterial infections entering through the teat canal. The main forms of mastitis are contagious (spreads from cow to cow) and environmental (from bedding, manure, etc.). Mastitis results in significant economic losses due to decreased milk production, treatment costs, and increased cow culling. While clinical mastitis shows visible signs like abnormal milk and udder inflammation, subclinical mastitis is more prevalent but only detectable through milk testing.