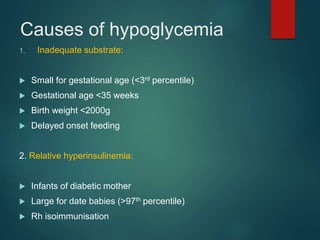
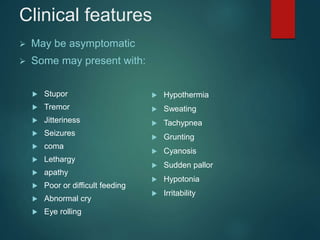
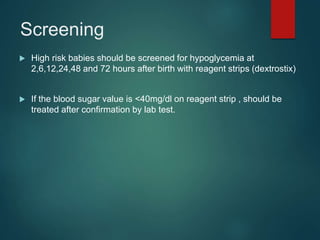
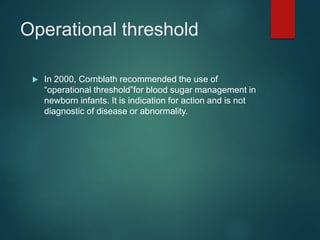
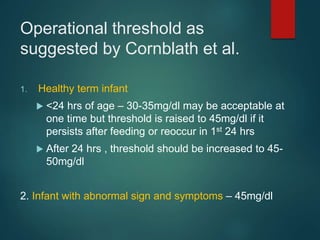
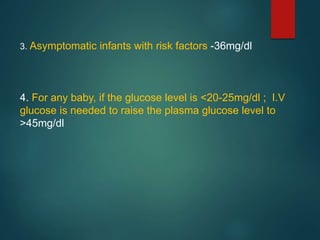
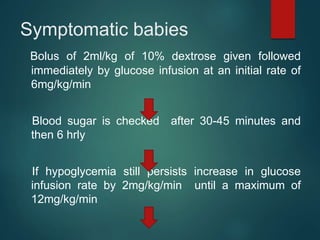
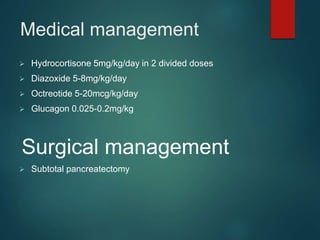
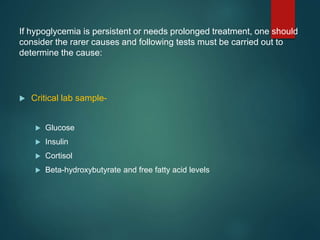
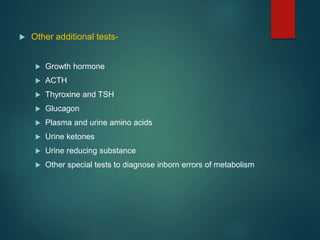
Neonatal hypoglycemia can be caused by inadequate substrate in small or preterm infants, relative hyperinsulinemia in infants of diabetic mothers or large babies, or sickness. Symptoms range from none to seizures or coma. High risk infants should be screened for blood glucose levels, with intervention if levels drop below thresholds. Asymptomatic infants with levels over 20mg/dL can be treated with frequent feeding and monitoring, while symptomatic infants receive IV glucose. Hypoglycemia management may also include medical treatments like hydrocortisone or diazoxide. Persistent cases require identifying underlying causes through additional laboratory tests and treatments.