The document provides an overview of lower respiratory tract infections, including pneumonia and pulmonary tuberculosis. It discusses various types of pneumonia such as community-acquired pneumonia, hospital-acquired pneumonia, and pneumonia in immunocompromised patients. For community-acquired pneumonia, it describes common causative agents and their characteristics. It also covers treatments for different types of pneumonia. The document additionally discusses pneumonia seen in immunocompromised individuals, including Pneumocystis pneumonia and fungal pneumonia.

![3. Hx of previous Rx pt registration group
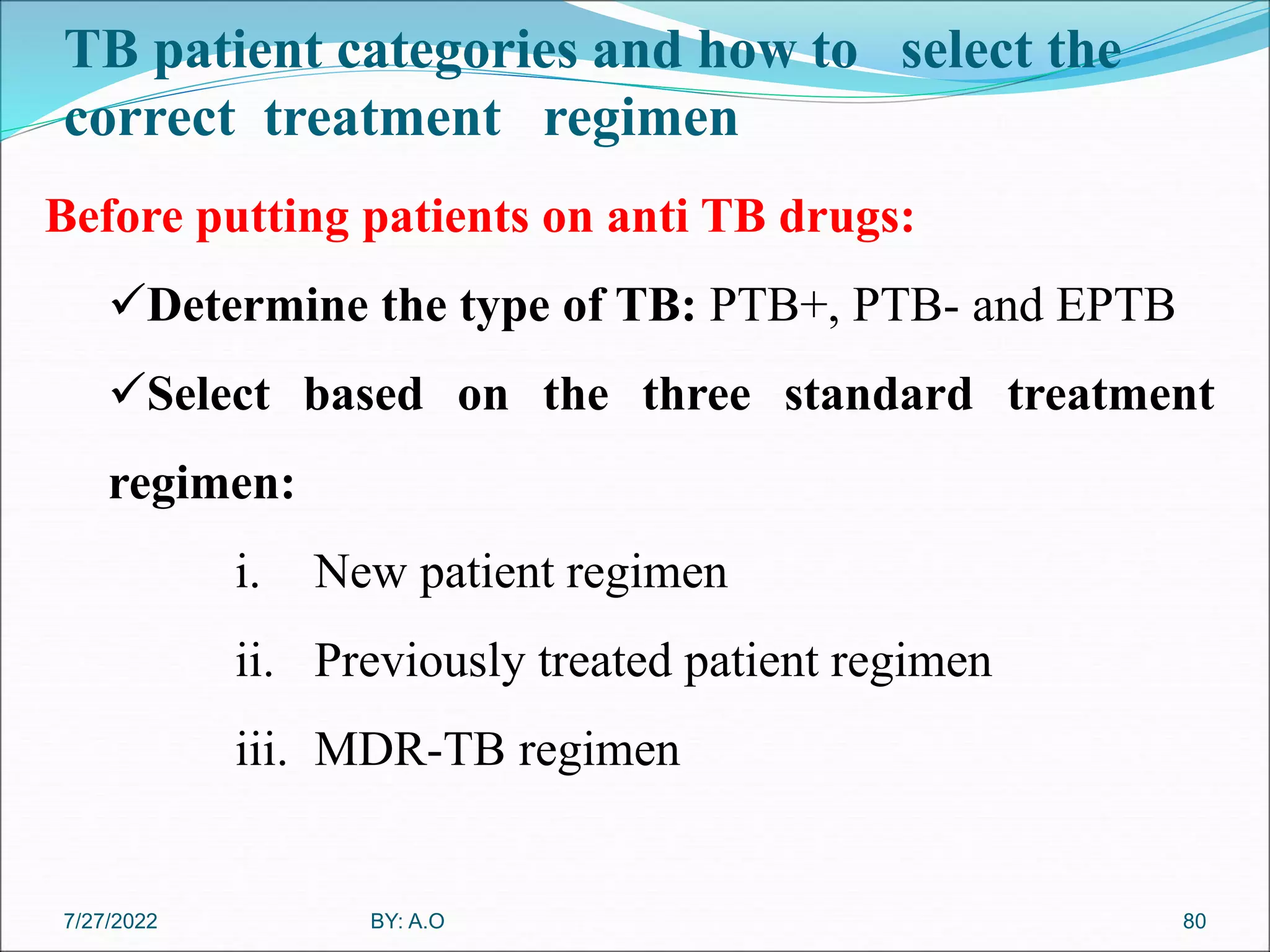
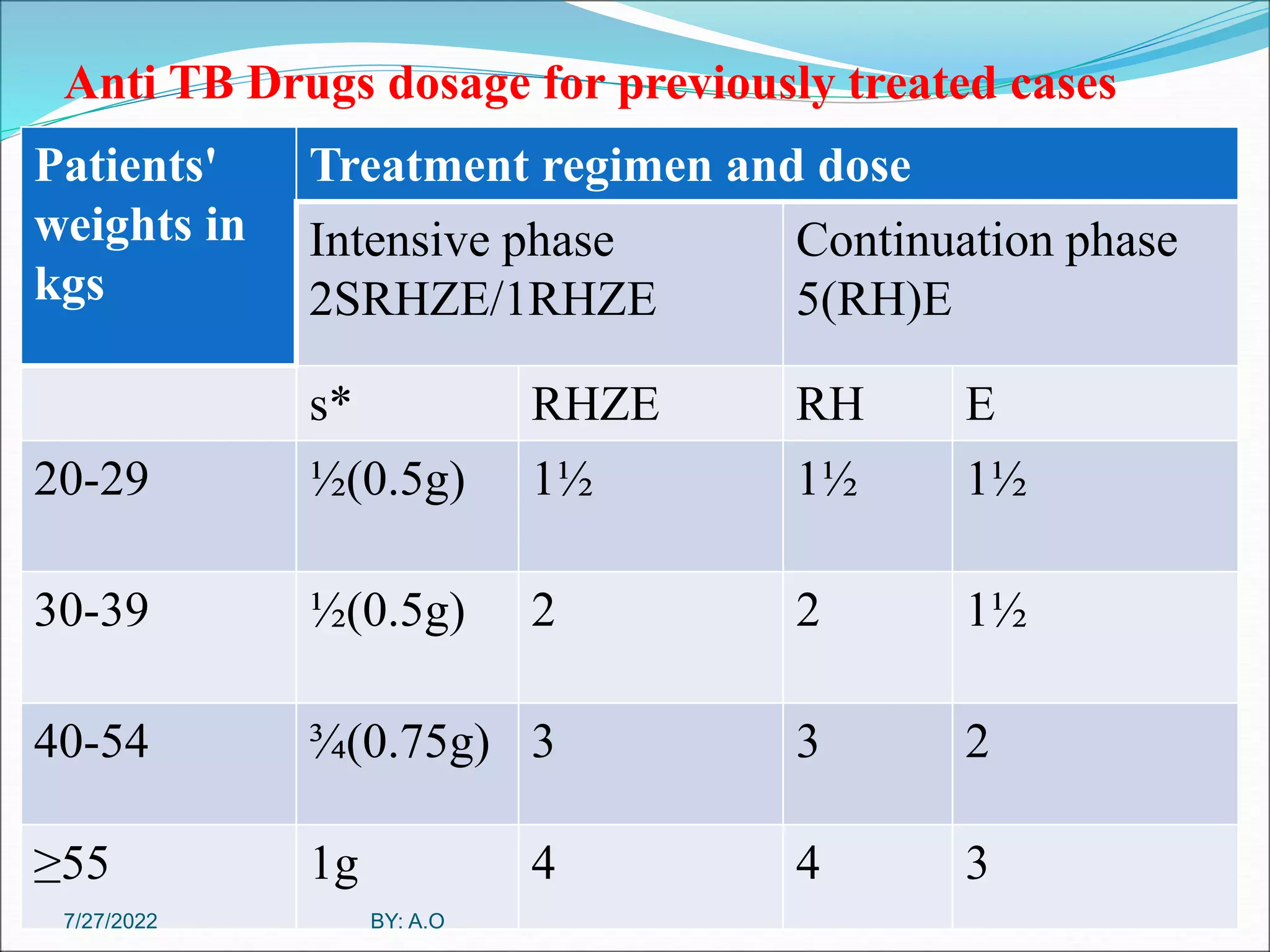
It is important to identify previously treated pt . B/c they
are high risk for drug resistance including MDR-TB.
New patient: A who never had Rx or have taken anti TB
for less than 1 month [New case (N)].
Previously Treated patient: A patient who have received
1 month or more of anti TB drug in the past& may have
+ve or –ve bacterlogical and may be any diseases at an
anatomical site .
67
BY: A.O
7/27/2022](https://image.slidesharecdn.com/lowerrespiratorydisorders2021updated-220727200023-e4d1e2e5/75/Lower-Respiratory-Disorders-2021-updated-ppt-67-2048.jpg)