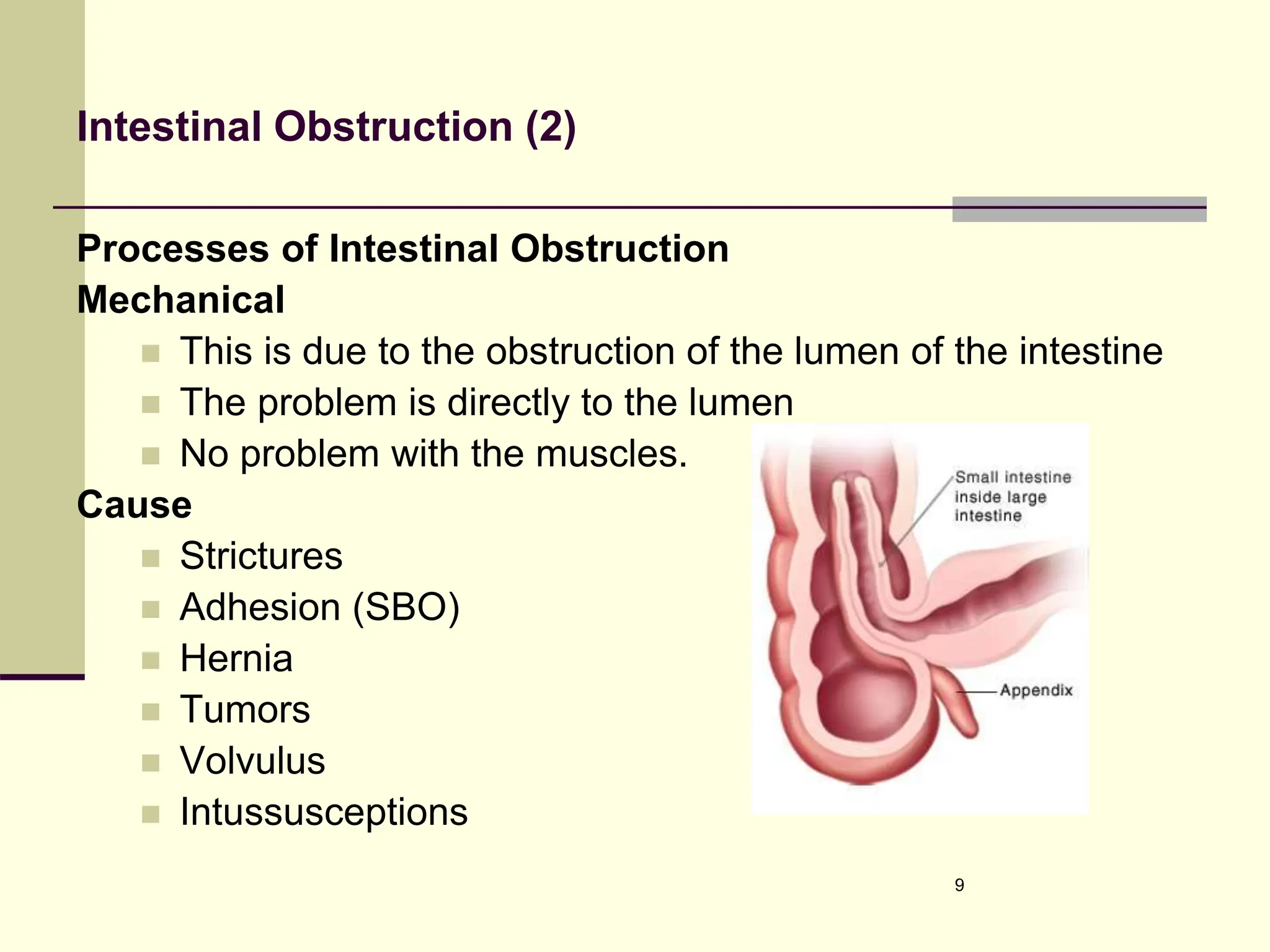
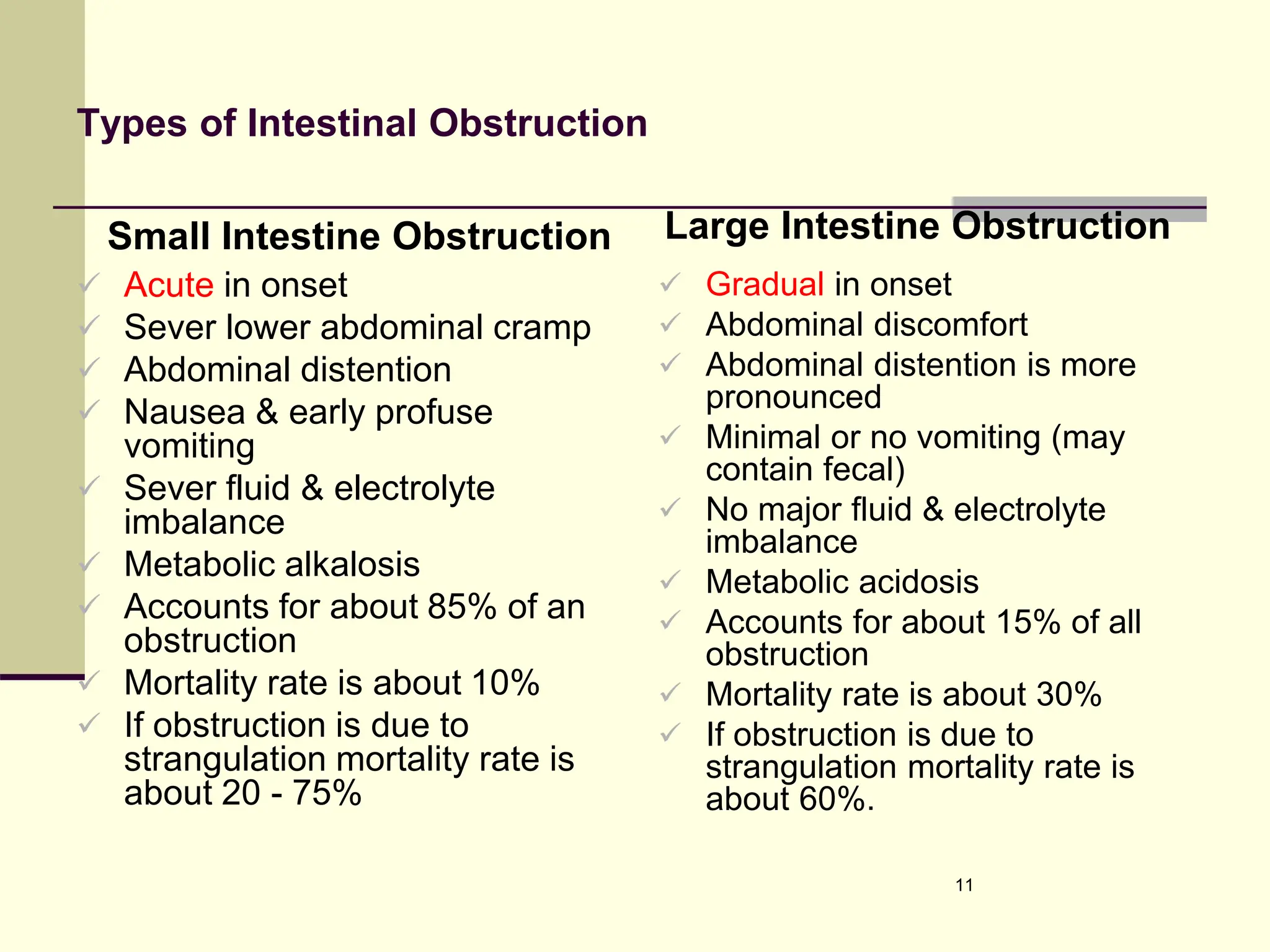
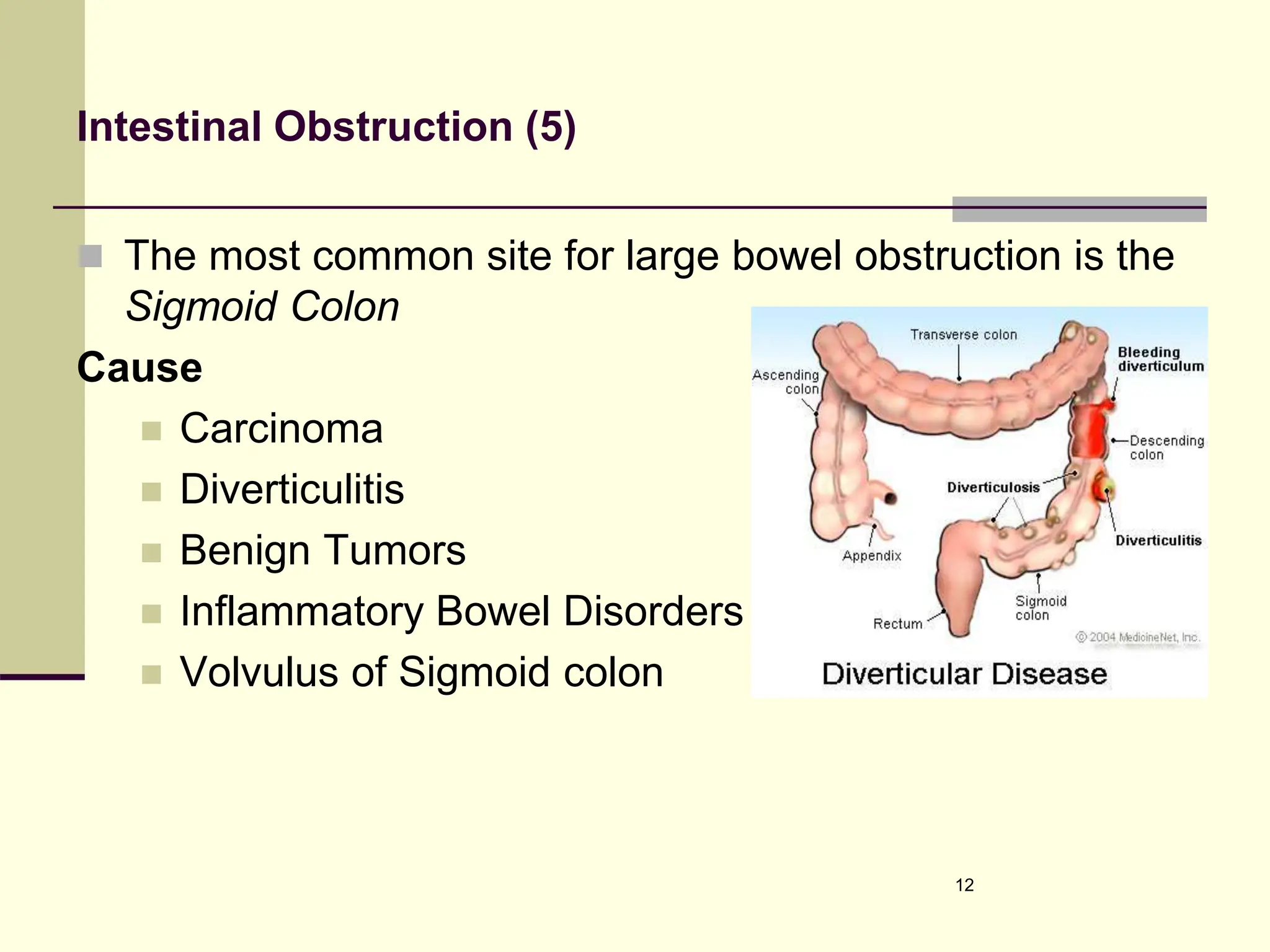
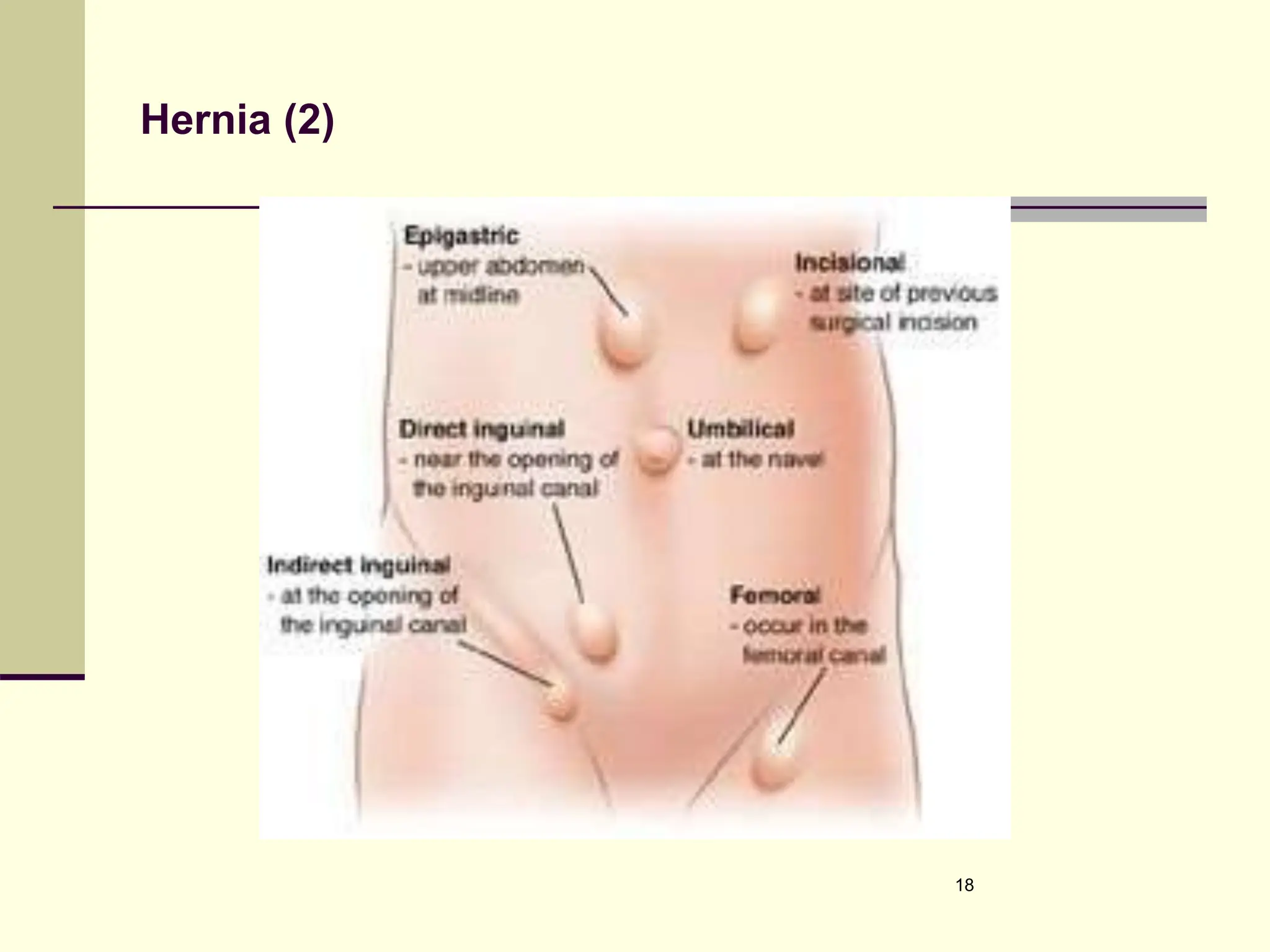
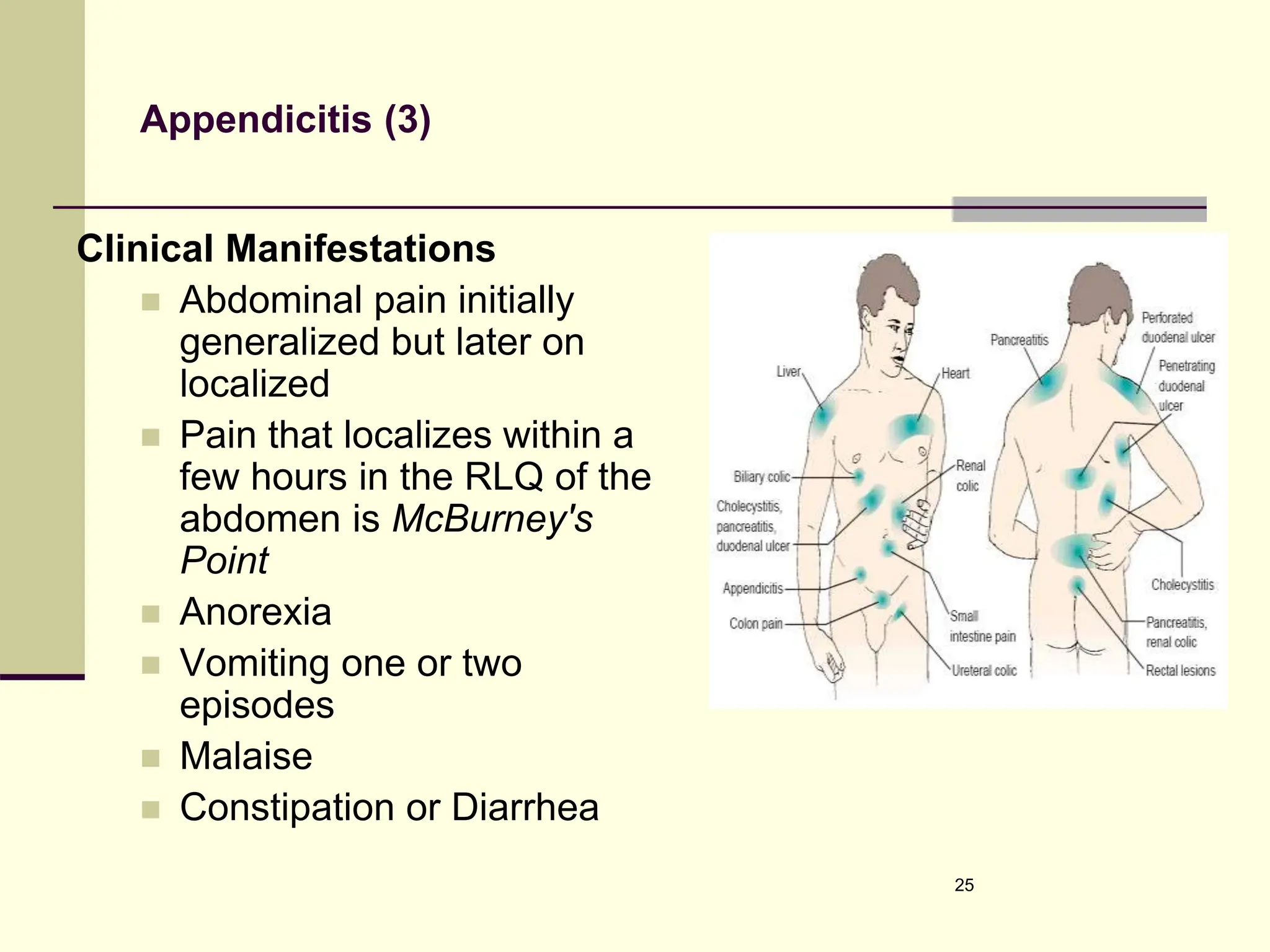
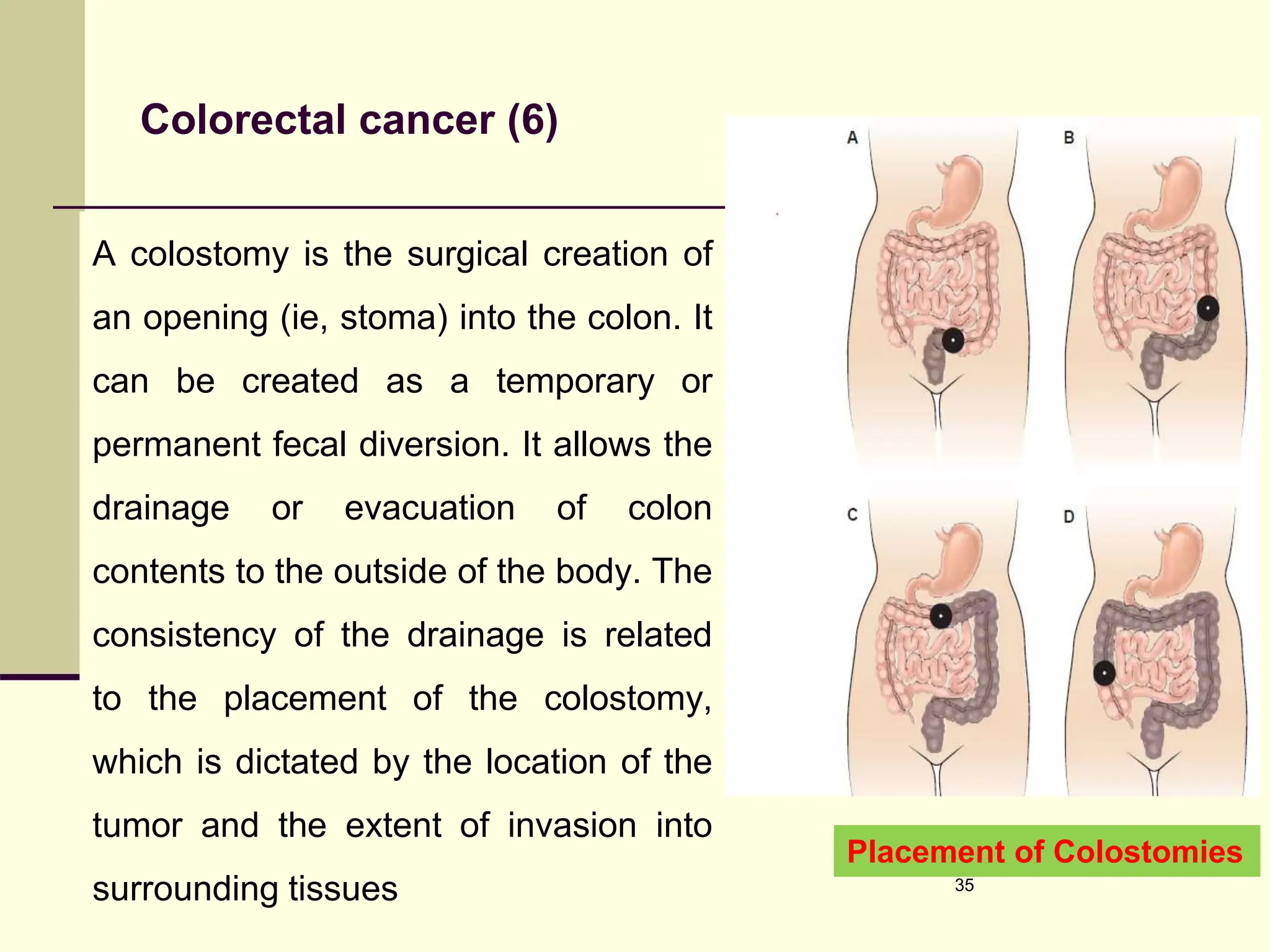
The document outlines nursing interventions for clients with lower gastrointestinal disorders, including constipation, diarrhea, intestinal obstruction, hernia, appendicitis, colorectal cancer, and hemorrhoids. Each condition is described with its clinical manifestations, medical management, nursing management, and complications. Important aspects like treatment options, dietary recommendations, and nursing interventions are highlighted to guide care for patients with these gastrointestinal issues.