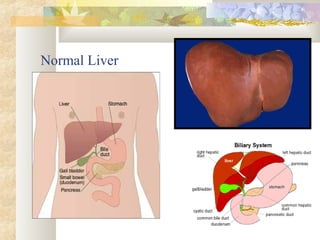
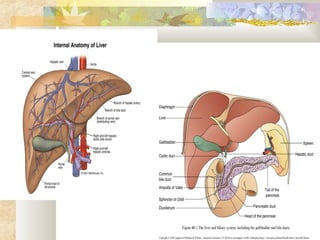
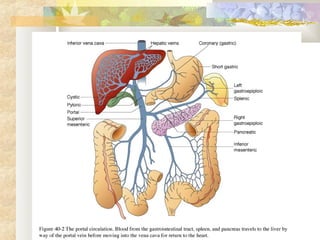
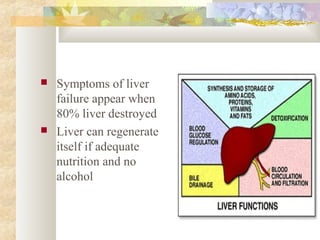
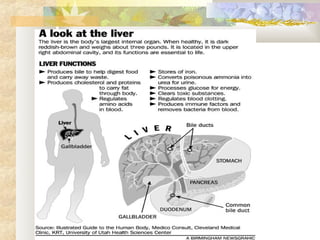
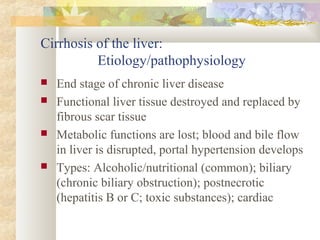
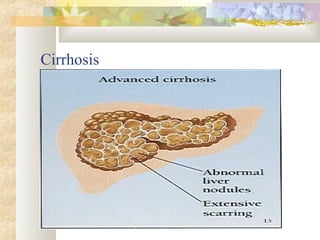
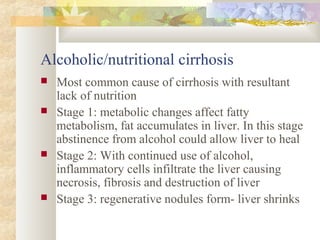
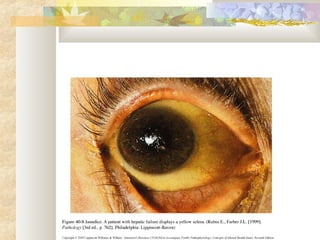
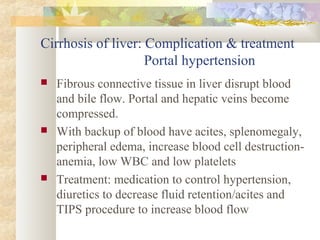
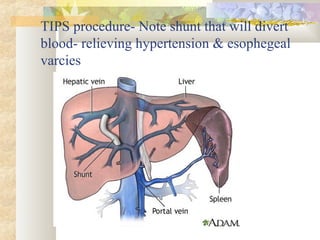
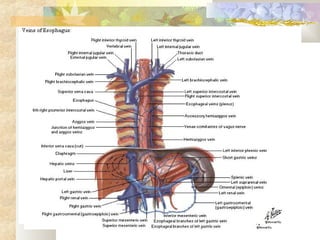
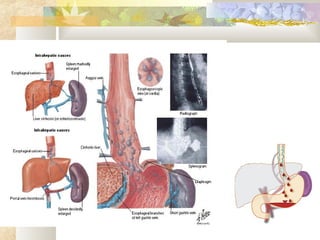
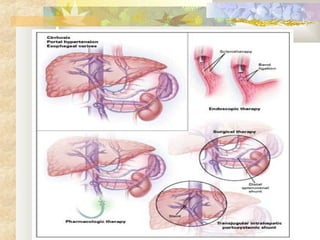
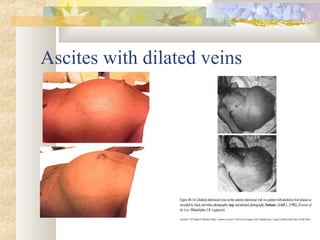
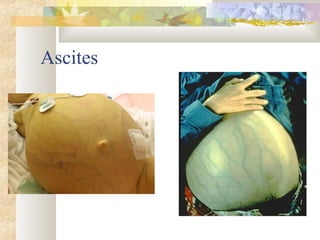
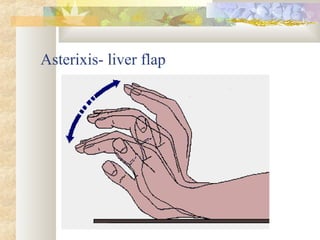
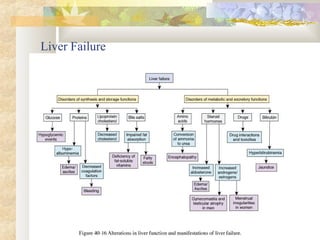
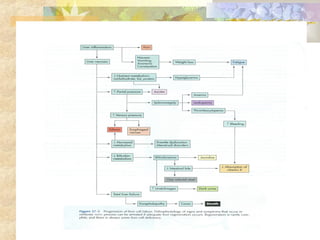
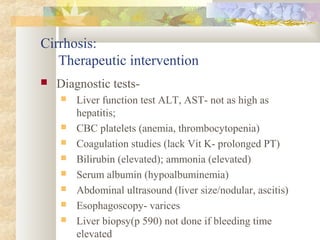
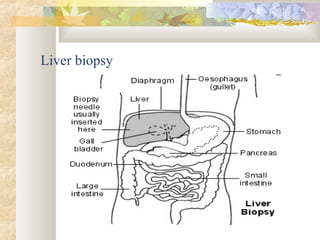
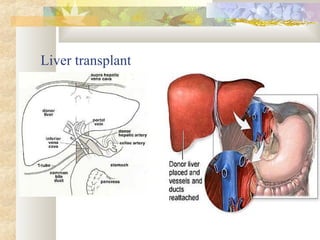
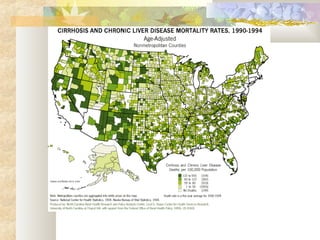
This document provides information about cirrhosis of the liver including its causes, stages of progression, complications, treatment, and nursing care considerations. Cirrhosis is the end stage of chronic liver disease where liver tissue is replaced by scar tissue, disrupting blood flow and metabolic functions. Common causes include alcoholism and hepatitis. Complications include portal hypertension, esophageal varices, ascites, and hepatic encephalopathy. Treatment focuses on managing complications, medications to reduce bleeding risk and ammonia levels, dietary changes, and potentially liver transplantation. Nursing care involves monitoring for symptoms, providing education, managing fluid balance and medications, and preventing complications.