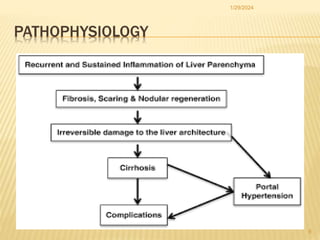
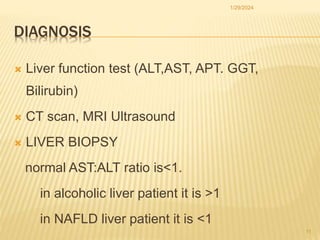
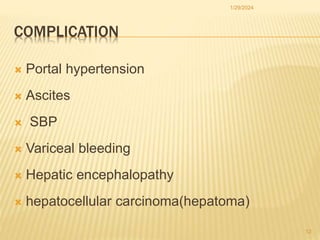
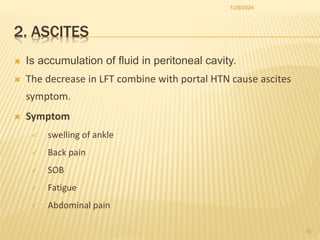
This document discusses chronic liver disease and provides details on its epidemiology, risk factors, etiology, pathophysiology, clinical presentation, diagnosis, complications, and treatment. It defines chronic liver disease as the progressive decline of liver function for more than six months. It describes the major causes as alcohol, viral infections like hepatitis B and C, and non-alcoholic fatty liver disease. Complications discussed include portal hypertension, ascites, spontaneous bacterial peritonitis, variceal bleeding, and hepatic encephalopathy.






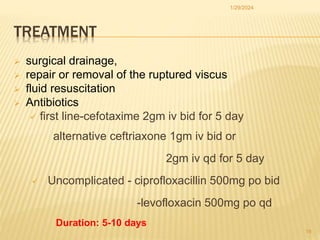
![3. SPONTANEOUS BACTERIAL PERITONITIS (SBP]
Is defined as bacterial infection of the ascetic fluid. Due to
enterobacteria or pneumococci
SBP is defined as ascetic fluid polymorph nuclear leukocyte (PMN)
count level ≥ 250 cells/µL without a surgical, intra-abdominal cause
of infection
Incidence: 10-30% of hospitalized patients with cirrhosis and ascites
Clinical presentation: Fever, abdominal pain, nausea, vomiting,
diarrhea, rebound tenderness, and exacerbation of encephalopathy
1/29/2024
18](https://image.slidesharecdn.com/cldemerseminareyael-240129080042-8b148c3f/85/CLD-EMER-SEMINAR-Eyael-pptx-18-320.jpg)