The document discusses liver function tests and their importance. It provides 3 key points:
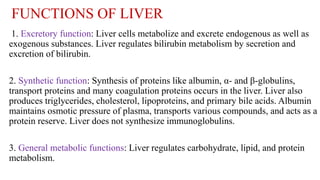
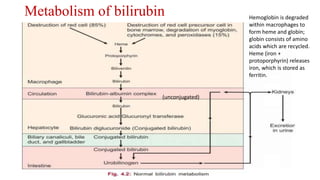
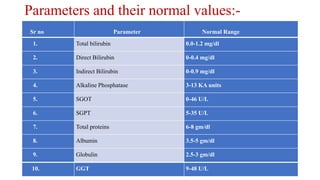
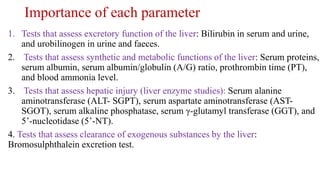
1. Liver function tests assess the excretory, synthetic, and metabolic functions of the liver such as bilirubin metabolism, protein and clotting factor synthesis, and carbohydrate/lipid processing.
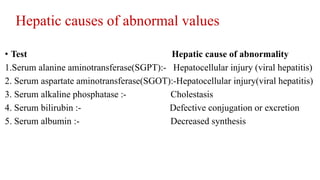
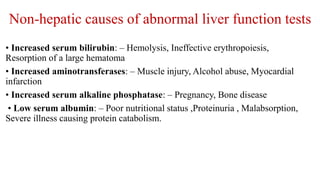
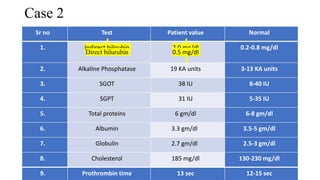
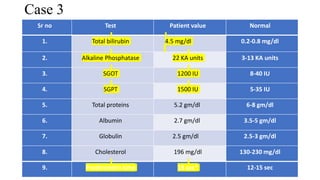
2. Elevated liver enzymes like ALT, AST, and ALP indicate liver injury or disease while abnormal protein and clotting tests reveal synthetic or metabolic dysfunction.
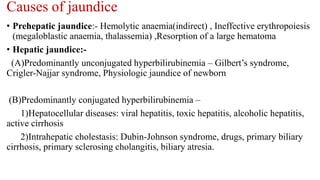
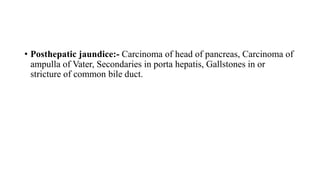
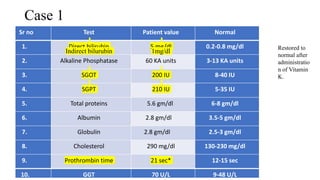
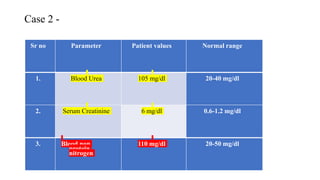
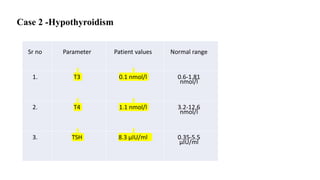
3. Case studies are presented to demonstrate how liver function test results can indicate specific liver conditions like obstruction, hepatitis, or hemolytic anemia.