Understanding Metabolic Syndrome in PCOS: Symptoms, Risks, and Management
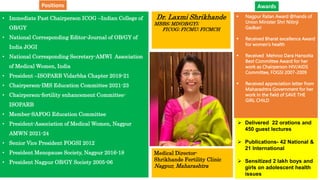
- 1. • Immediate Past Chairperson ICOG –Indian College of OB/GY • National Corresponding Editor-Journal of OB/GY of India JOGI • National Corresponding Secretary-AMWI Association of Medical Women, India • President –ISOPARB Vidarbha Chapter 2019-21 • Chairperson-IMS Education Committee 2021-23 • Chairperson-fertility enhancement Committee- ISOPARB • Member-SAFOG Education Committee • President-Association of Medical Women, Nagpur AMWN 2021-24 • Senior Vice President FOGSI 2012 • President Menopause Society, Nagpur 2016-18 • President Nagpur OB/GY Society 2005-06 Dr. Laxmi Shrikhande MBBS; MD(OB/GY); FICOG; FICMU; FICMCH Medical Director- Shrikhande Fertility Clinic Nagpur, Maharashtra Nagpur Ratan Award @hands of Union Minister Shri Nitinji Gadkari Received Bharat excellence Award for women’s health Received Mehroo Dara Hansotia Best Committee Award for her work as Chairperson HIV/AIDS Committee, FOGSI 2007-2009 Received appreciation letter from Maharashtra Government for her work in the field of SAVE THE GIRL CHILD Delivered 22 orations and 450 guest lectures Publications- 42 National & 21 International Sensitized 2 lakh boys and girls on adolescent health issues Awards Positions
- 2. Metabolic Syndrome in Women with PCOS Dr Laxmi Shrikhande Consultant –Shrikhande Hospital & Research Centre Nagpur
- 4. Introduction Polycystic ovary syndrome (PCOS) affects 10–18% of women of reproductive age. Insulin resistance (IR) appears to be important in the pathogenesis of PCOS and subsequent metabolic syndrome. The prevalence of metabolic syndrome is as high as 33% in women with PCOS, and is associated with long-term consequences such as cardiovascular disease (CVD), diabetes type II, cancers, sleep apnoea and psychological problems. Conventionally, management of PCOS has focused on infertility, anovulation and hirsutism; thus, there is a need to increase clinicians’ awareness of metabolic syndrome. The enormity of the health burden of metabolic syndrome means that accurate identification and timely intervention are extremely important.
- 5. PCOS - Late sequelae Diabetes mellitus x7 Hypertension x4 Low HDL/high LDL Endometrial Cancer
- 7. Insulin resistance IR and its consequent hyperinsulinemia, is central to the pathogenesis of PCOS. Insulin regulates metabolic and mitogenic pathways that function independent of each other. This might explain the paradoxical insulin sensitivity patterns seen in different tissues, for example, resistance in peripheral tissues and retained sensitivity in the ovarian cortex. Metabolic inertia to insulin has been attributed to a post-binding defect in the insulin signalling pathway caused by abnormal serine phosphorylation of the insulin receptor. Despite extensive data supporting the role of IR, it remains unclear whether the association is causal, propagative or merely co-existential. Cusi K, Maezono K, Osman A, Pendergrass M, Patti ME, Pratipanawatr T,et al. Insulin resistance differentially affects the PI 3- kinase- and MAPkinase-mediated signaling in human muscle. J Clin Invest 2000;105:311–20.
- 8. Atherogenic dyslipidaemia In adipocytes, IR leads to the increased shunting of free fatty acids (FFA) from fat tissue to the liver. FFAs induce hepatic synthesis of very low-density lipoprotein (VLDL), resulting in elevated triglycerides and apolipoprotein B and decreased HDL. These alterations in lipid parameters lead to atherogenic dyslipidaemia. PCOS is associated with chronic low-grade systemic inflammation, which mediates insulin resistance and accelerates atherogenesis. Besides genetic abnormalities, obesity and a high glycaemic diet are also known to induce pro-inflammatory cytokines such as tumour necrosis factor alpha (TNFa) and interleukin-6 (IL-6). Aubuchon M, Jennifer A. Bickhaus, Gonzalez F. Obesity, metabolicdysfunction and inflammation in polycystic ovary syndrome. In: Pal Lubna, editor. Polycystic Ovary Syndrome. New York: Springer; 2014. p.117–44. Moran LJ, Noakes M, Clifton PM, Tomlinson L, Galletly C, Norman RJ.Dietary composition in restoring reproductive and metabolic physiology in overweight women with polycystic ovary syndrome. J Clin Endocrinol Metab 2003;88:812–9. Thathapudi S, Kodati V, Erukkambattu J, Katragadda A, Addepally U, HasanQ. Tumornecrosis factor-alpha and polycystic ovarian syndrome: aclinical, biochemical, and molecular genetic study. Genet Test Mol Biomark 2014;18:605–9.
- 9. Obesity Obesity is known to perpetuate PCOS. It most likely results from the combined effect of genetic predisposition, poor diet and a sedentary lifestyle, thus compounding pre-existing metabolic derangements. Hyperinsulinemia, and the increased responsiveness of the ovarian theca to insulin, causes an increase in the levels of free androgens. Hyperandrogenaemia increases a person’s predilection for central adiposity and worsens insulin resistance and dyslipidaemia. Escobar-Morreale HF, San Millan JL. Abdominal adiposity and the polycystic ovary syndrome. Trends EndocrinolMetab 2007;18:266–72.
- 10. Hypertension In obese individuals, hypertension is linked to the potentiation of sympathetic outflow and the renin– angiotensin–aldosterone system, resulting from increased levels of insulin and free fatty acids. Concomitant vascular endothelial dysfunction also contributes to the development of hypertension. Analysing all available data on the aetiopathogenesis of PCOS, it is evident that a paradigm shift has taken place in our understanding of metabolic syndrome in PCOS, from mere ovarian dysfunction to a multisystemic, multifactorial aberration with far greater metabolic consequences than initially implicated. Rahmouni K, Correia MLG, Haynes WG, Mark AL. Obesityassociated hypertension: new insights into mechanisms. Hypertension2005;45:9–14.
- 11. Cardiovascular disease One meta-analysis demonstrated that in women with PCOS, the risk of coronary heart disease (CHD) and stroke is doubled. Despite adjusting for body mass index (BMI), there was a 55% increase in risk. Subjects with metabolic syndrome are three to six times more likely to develop CHD, with a 12% increase in mortality. Where metabolic syndrome coexists with PCOS, one would expect this risk to be significantly higher. Large-scale prospective studies that evaluate long-term outcomes are required to assess the magnitude of the impact of metabolic syndrome with PCOS on cardiovascular events. de Groot PCM, Dekkers OM, Romijn JA, Dieben SWM, Helmerhorst FM.PCOS, coronary heart disease, stroke and the influence of obesity: a systematic review and meta-analysis. Hum Reprod Update 2011;17:495– 500. Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001;24:683–9.
- 12. Diabetes Metabolic syndrome confers a five-fold increase in risk for diabetes type II, and PCOS has been identified as a significant non-modifiable risk factor. Women with PCOS with baseline normoglycaemia have a more pronounced risk of developing impaired glucose tolerance (IGT); up to 16% of women with PCOS convert to IGT per year. Women with baseline IGT have a 2% risk of progressing to diabetes type II per year, and over 6 years this risk maybe as high as 54%. A meta-analysis on the impact of PCOS on reproductive outcomes has shown a three-fold increase in risk for gestational diabetes. Legro RS, Gnatuk CL, Kunselman AR, Dunaif A. Changes in glucose tolerance over time in women with polycystic ovary syndrome: a controlled study. J Clin Endocrinol Metab 2005;90:3236–42. Norman RJ, Masters L, Milner CR, Wang JX, Davies MJ. Relative risk of conversion from normoglycaemia to impaired glucose tolerance or noninsulin dependent diabetes mellitus in polycystic ovarian syndrome. Hum Reprod 2001;16:1995–8. Boomsma CM, Eijkemans MJC, Hughes EG, Visser GHA, Fauser BCJM, Macklon NS. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum Reprod Update 2006;12:673–83.
- 13. Cancers PCOS is associated with an increased likelihood of endometrial cancer (odds ratio [OR] 2.89). However, it is difficult to ascertain the independent effect of PCOS because of the additive influence of diabetes, hypertension, obesity, chronic anovulation and hyperestrogenaemia on the development of endometrial cancer. There is no strong association between PCOS and ovarian or breast cancer. Metabolic syndrome has been associated with an increased risk of endometrial cancer (OR 1.6) and a higher incidence of pancreatic, postmenopausal breast and colorectal cancers (OR 1.5). Poorer cancer outcomes, increased recurrences and overall mortality have also been linked to metabolic syndrome. Chittenden BG, Fullerton G, Maheshwari A, Bhattacharya S. Polycystic ovary syndrome and the risk of gynaecological cancer: a systematic review. Reprod Biomed Online 2009;19:398–405. Royal College of Obstetricians and Gynaecologists. Long-term consequences of polycystic ovarian syndrome. Green-top Guideline No. 33. London: RCOG; 2007 [https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_33.pdf].
- 14. Obstructive sleep apnoea PCOS is associated with up to a 30-fold higher risk of obstructive sleep apnoea (OSA), and a nine-fold increase in excessive daytime sleepiness. IR has emerged as a principal predictor for the risk of OSA, independent of elevated testosterone levels and obesity. The presence of OSA in metabolic syndrome in turn worsens IR and cardiovascular outcomes. Women should be screened for and counselled about snoring, daytime somnolence and fatigue, and offered interventions when necessary. Vgontzas AN, Bixler EO, Chrousos GP. Sleep apnea is a manifestation of the metabolic syndrome. Sleep Med Rev 2005;9:211–24.
- 15. Psychological problems The prevalence of depression is higher in women with PCOS (OR 4.03) than the general population, with increased severity of symptoms. This association is independent of BMI. These women are also more likely to develop anxiety, eating disorders and dysfunctional relationships. Metabolic syndrome is associated with depression, mainly with neurovegetative features such as fatigue. Although inflammation has been linked to the development of depressive symptoms, the precise mechanisms have yet to be elucidated. Since these factors significantly affect quality of life, it is essential to screen women for symptoms and to refer them to a specialist when required. Dokras A, Clifton S, Futterweit W, Wild R. Increased risk for abnormal depression scores in women with polycystic ovary syndrome: a systematic review and meta-analysis. Obstet Gynecol 2011;117:145–52. Capuron L, Su S, Miller AH, Bremner JD, Goldberg J, Vogt GJ, et al. Depressive symptoms and metabolic syndrome: is inflammation the
- 16. Diagnostic criteria Metabolic syndrome was first identified as a clinical entity with insulin resistance central to its pathogenesis. Thus, historically, the definition of metabolic syndrome mandated the presence of IR for its diagnosis. Subsequent definitions included more composite criteria; for example, waist circumference as a measure of central obesity. Multiple definitions for metabolic syndrome have been proposed over the years, reflecting a shift in the proposed pathogenetic mechanisms and clinical implications .
- 17. Definition However, so far several definitions have been proposed by World Health Organi-zation (WHO), The International Disease Federation (IDF), The National Cholesterol Education Program (NCEP), and American Heart Association (AHA) National Heart, Lung and Blood Institute (NHLBI)) “Adult Treatment Panel III (ATP III)”- has been widely used as a common definition in literature Grundy, S.M., Brewer Jr., H.B., Cleeman, J.I., et al. (2004) Definition of Metabolic Syndrome: Report of the National Heart, Lung and Blood Institute/American Heart Association Conference on Scientific Issues Related to Definition. Circulation, 109, 433-438.
- 18. Diagnostic Criterias High waist circumference (WC > 102 cm in men and WC > 88 cm in women), High blood pressure (BP > 130/80 mm/Hg), High triglyceride (TG > 150 mm/dl), High glucose (FBG > 110 mg/dl, and Low HDL (HDL < 40 mg/dl in men and HDL < 50 mg/dl in women)
- 19. The Obstetric & Gynaecologis, Volume: 20, Issue: 4, Pages: 245-252, First published: 20 July 2018, DOI: (10.1111/tog.12519) Figure 1. Diagnosis of metabolic syndrome. Key: NCEP:ATP III = National Cholesterol Education Program Adult Treatment Panel III;24 AHA/NHLBI = the American Heart Association/ National Heart, Lung, and Blood Institute;25 IDF = International Diabetes Federation;26 JIS = Joint Interim Statement.27
- 20. The definition of metabolic syndrome The definition of metabolic syndrome proposed by the National Cholesterol Education Program Adult Treatment Panel III (NCEP:ATP III) does not build on any preconceived notion about the underlying cause(s) of metabolic syndrome, whether insulin resistance or obesity. In 2005, the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) statement incorporated a minor modification to that of the NCEP: ATP III by revising the fasting blood glucose cut-off to 5.6 mmol/l. In the USA, the NCEP:ATP III recommends 88 cm as a cut-off for waist circumference in women. This is in contrast to the International Diabetes Federation (IDF), which focuses on the impact of ethnic differences on the threshold for abdominal obesity and makes it obligatory to the definition. Data analysed by the IDF supports a waist circumference of 80 cm and higher in women across different ethnicities. The Joint Interim Statement (JIS), however, highlighted the importance of ethnicity- specific waist measurements, with equal emphasis placed on the individual risk-predicting factors. By unifying the diagnostic criteria of metabolic syndrome, the JIS simplifies its utility as a clinical tool and has emerged as one of the most commonly used definitions. Grundy SM, Cleeman JI, Daniels SR, et al. American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735–52. Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome–a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med J Br Diabet Assoc 2006;23:469–80. Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International
- 21. Screening for metabolic syndrome A structured assessment for the early detection and management of metabolic syndrome, especially in women of reproductive age, would be of critical importance to the healthcare system. So that it can be applied in the clinical setting, this assessment would need to prioritise risks, standardise evaluation methods, and establish the frequency of further testing. A comprehensive evaluation of the risk factors for metabolic syndrome, adapted from evidence based guidelines from Australia and the UK’s Royal College of Obstetricians and Gynaecologists is shown in Table 2. Teede HJ, Misso ML, Deeks AA, Moran LJ, Stuckey BG, Wong JL, et al. Assessment and management of polycystic ovary syndrome: summary of an evidence-based guideline. Med J Aust 2011;195:S65–112
- 22. Table 2. Recommendations for metabolic syndrome risk factor screening in women with polycystic ovary syndrome Screening parameters Frequency of assessment Cigarette smoking Obesity (weight, BMI, waist circumference) Blood pressure At every visit, obtain history of recent smoking habits, if any, or cessation At every visit Complete lipid profile Oral glucose tolerance test (75 g) For women with a BMI <25 kg/m2: annually For women with a BMI ≥25 kg/m2: at every visit For women with a normal profile: every 2 years For women with an abnormal profile or excess weight: annually All women: every 2 years Women with risk factors (age >40 years, ethnicity, physical inactivity, smoking, waist circumference (>80 cm), BMI ≥25 kg/m2, hypertension, previous gestational diabetes mellitus, family history of diabetes mellitus): annually Key: BMI = body mass index
- 23. Management With metabolic syndrome adding to the burgeoning epidemic of diabetes type II and CVD, instituting early and targeted interventions is a medical exigency. Primary intervention for metabolic syndrome requires adopting lifestyle changes that may prevent or slow progression to adverse events in high-risk individuals. In those who do not respond adequately to lifestyle modifications, secondary interventions can be considered, including drug therapy and bariatric surgery.
- 24. Lifestyle modifications Exercise and dietary regulation are important components of a healthy lifestyle. Though there is no established cure for PCOS, lifestyle changes have demonstrated substantial improvements in symptoms. It is recommended that women with PCOS aim to lose 5–10% of their body weight in the first year after diagnosis for improved clinical outcomes. Reduced body weight is associated with a decrease in metabolically active visceral fat, which in turn leads to decreased insulin resistance and an optimised lipid profile, and may have psychological benefits such as reduced anxiety and depression. The heterogeneity of study designs means that the optimal duration, frequency and type of exercise is difficult to establish based on currently available data. To improve cardiometabolic outcomes, women with PCOS are recommended to undertake regular exercise for 150 minutes per week, which should include at least 90 minutes of moderate-intensity aerobic activity. Alberti KGM, Zimmet P, Shaw J. The metabolic syndrome – a new worldwide definition. Lancet 2005;366:1059–62. Harrison CL, Lombard CB, Moran LJ, Teede HJ. Exercise therapy in polycystic ovary syndrome: a systematic review. Hum Reprod Update
- 25. Lifestyle modifications There are several elements that can be optimised in terms of dietary goals: the quality, quantity and spacing of meals. In obese women with PCOS, incorporating carbohydrates with a low glycaemic index (GI) has demonstrated considerable improvement in insulin sensitivity. Dietary fibre is the indigestible part of food that causes satiety, lowers cholesterol and slows absorption of carbohydrates. Proteins take longer to digest than carbohydrates, hence they can improve the insulin profile. Monounsaturated fatty acids improve cholesterol and glucose levels, as well as insulin response. Very long chain polyunsaturated fatty acids, including omega-3 and omega-6 fats have a hypotriglyceridaemic effect and may ameliorate inflammation in metabolic syndrome. Adequate omega-3 fat intake is important in PCOS; benefits include lower levels of inflammatory markers, cholesterol and triglycerides and increased insulin sensitivity. To maximise the benefits of a healthy diet, it is also important to adopt healthy eating patterns, for example, taking small portions of calorie-appropriate meals at frequent intervals. Marsh KA, Steinbeck KS, Atkinson FS, Petocz P, Brand-Miller JC. Effect of a low glycemic index compared with a conventional healthy diet on polycystic ovary syndrome. Am J Clin Nutr 2010;92:83–92. Krystock A. Role of lifestyle and diet in the management of polycysticovarian syndrome. In: Pal L, editor. Polycystic Ovary Syndrome: Current and Emerging Concepts. New York: Springer-Verlag; 2014. p. 147–64.
- 26. Metabolic syndrome in women with polycystic ovary syndrome The Obstetric & Gynaecologis, Volume: 20, Issue: 4, Pages: 245-252, First published: 20 July 2018, DOI: (10.1111/tog.12519)
- 27. Medical management Insulin-sensitising agents Metformin Metformin improves insulin sensitivity in women with PCOS. It has also been shown to decrease fasting insulin levels, but this benefit was restricted to non-obese women with PCOS (BMI <30 kg/m2). There is no robust evidence for the use of metformin to merely ameliorate insulin resistance associated with PCOS, and its use to combat the same in normoglycaemic women is not recommended by any international organisation. Women with IGT have a significant risk of conversion to diabetes type ll. Metformin can be considered for use in women with IGT to prevent progression to diabetes type II, although this requires further scientific validation. Metformin has been used in incremental doses ranging from 500 to 1500 mg/day. There is no consensus on the duration of treatment required. It is commonly associated with adverse gastrointestinal effects, including nausea, abdominal pain and diarrhoea. A few trials have demonstrated that use of metformin can lead to significant weight loss, especially when combined with lifestyle modifications, but there is insufficient evidence to recommend its use for weight loss purposes. Moghetti P, Castello R, Negri C, Tosi F, Perrone F, Caputo M, et al. Metformin effects on clinical features, endocrine and metabolic profiles, and insulin sensitivity in polycystic ovary syndrome: a randomized, doubleblind, placebo-controlled 6-month trial, followed by open, long-term clinical evaluation. J Clin Endocrinol Metab 2000;85:139–46. Tang T, Lord JM, Norman RJ, Yasmin E, Balen AH. Insulin-sensitising drugs (metformin, rosiglitazone, pioglitazone, D-chiro-inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility. Cochrane Database Syst Rev 2012;(5):CD003053. Pasquali R, Gambineri A, Biscotti D, Vicennati V, Gagliardi L, Colitta D, et al. Effect of long-term treatment with metformin added to hypocaloric diet on body composition, fat
- 28. Inositol MI and DCI are involved in downstream signalling pathways following the activation of insulin receptors and are considered mediators of insulin action. Various studies have demonstrated that administration of DCI leads to decreased basal insulin levels, an improved lipid profile and reduced systolic blood pressure. The clinical effectiveness of MI and DCI has been studied in combination and as standalone interventions, with MI being administered at doses ranging from 1 to 4 g/day. No appreciable adverse effects have ever been recorded following the administration of inositols. Preliminary data suggest that supplementing with inositol can be considered for improving a patient’s metabolic profile, but more studies are required before its use can be standardised. Croze ML, Soulage CO. Potential role and therapeutic interests of myoinositol in metabolic diseases. Biochimie 2013;95:1811–27. Costantino D, Minozzi G, Minozzi E, Guaraldi C. Metabolic and hormonal effects of myo-inositol in women with polycystic ovary syndrome: a double blind trial. Eur Rev Med Pharmacol Sci 2009;13:105–10. Genazzani AD, Lanzoni C, Ricchieri F, Jasonni VM. Myo-inositol administration positively affects hyperinsulinemia and hormonal parameters in overweight patients with polycystic ovary syndrome. Gynecol Endocrinol 2008;24:139–44. Zeng L, Yang K. Effectiveness of myoinositol for polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine 2018;59:30–8. Sortino MA, Salomone S, Carruba MO, Drago F. Polycystic ovary syndrome: insights into the therapeutic approach with inositols. Front Pharmacol 2017;8:341.
- 29. Anti-obesity agents-Orlistat Orlistat, rimonabant and sibutramine have been used in the pharmacotherapy of obesity in PCOS. Sibutramine and rimonabant have been withdrawn over safety concerns. Orlistat is an irreversible gastric lipase inhibitor that prevents the breakdown of dietary fat and thus, its absorption. In PCOS, orlistat induces significant and sustainable weight loss with similar efficacy to metformin. Its use is also associated with an improved lipid profile, including significant reductions in the levels of total cholesterol, low-density lipoprotein and triglycerides. Based on available evidence, orlistat can be considered for the treatment of overweight and obese women with PCOS for whom lifestyle modifications are insufficient. Patients take 60–360 mg of orlistat per day, divided between two to three doses. Its use is associated with mild to moderate gastrointestinal side effects including steatorrhoea and abdominal pain, which potentially affects compliance to treatment. Panidis D, Tziomalos K, Papadakis E, Vosnakis C, Chatzis P, Katsikis I. Lifestyle intervention and anti-obesity therapies in the polycystic ovary syndrome: impact on metabolism and fertility. Endocrine 2013;44:583–90.
- 30. Anti-obesity agents-Orlistat A randomised study on the effect of orlistat on obese women with metabolic syndrome demonstrated reversal of metabolic syndrome in 43.5% of participants, with associated significant improvements in anthropometry, insulin resistance, lipid profile and blood pressure.46 The risk of progression of IGT to diabetes type II was also significantly reduced (by 37.3%). Extending this favourable effect to cardiovascular risk, orlistat might have a role in the management of metabolic syndrome. However, further studies are required to assess the use of orlistat in women with PCOS and metabolic syndrome before it can be approved for therapeutic indications. Filippatos TD, Kiortsis DN, Liberopoulos EN, Georgoula M, Mikhailidis DP, Elisaf MS. Effect of orlistat, micronisedfenofibrate and their combination on metabolic parameters in overweight and obese patients with the metabolic syndrome: the FenOrli study. Curr Med Res Opin 2005;21:1997– 2006. Torgerson JS, Hauptman J, Boldrin MN, Sj€ostr€om L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a
- 31. Anti-obesity agents- Liraglutide Glucagon-like peptide receptor agonists (GLP-1R), including exenatide and liraglutide, are approved antiobesity agents. The use of liraglutide for obesity in PCOS related metabolic syndrome remains limited. Administration of liraglutide is associated with a significant reduction in BMI (–1.65 kg/m2), but not in waist:hip ratio, which is a more sensitive indicator of visceral obesity and metabolic outcomes. No significant positive effect has been shown on fasting insulin levels and insulin resistance. The use of liraglutide is limited by the need for parenteral administration, and the frequent occurrence of gastrointestinal adverse effects. Larger studies are required to establish the efficacy of GLP-1R agonists in women with PCOS and metabolic syndrome. Niafar M, Pourafkari L, Porhomayon J, Nader N. A systematic review of GLP-1 agonists on the metabolic syndrome in women with polycystic ovaries. Arch Gynecol Obstet 2016;293:509–15.
- 32. Anti-obesity agents-newer drug Semaglutide Tablets /Inj • In 2021, the FDA approved the semaglutide-containing medication for chronic weight management in adults with obesity or overweight with at least one weight-related condition.13 Mar 2024
- 33. Statins In women with dyslipidaemia, the use of statins results in significantly and consistently improved lipid profiles. Furthermore, reduced levels of markers of endothelial dysfunction and systemic inflammation suggest a decrease in cardiovascular risk factors. Although statins seem to create a favourable metabolic environment, their use is limited by certain risks. Long-term use can cause liver dysfunction and, when prescribed with other drugs, can lead to serious adverse effects, including teratogenicity, which is of critical concern among women of reproductive age. Based on available evidence, the routine clinical use of statins cannot be recommended for women with PCOS. Although there appear to be multiple options for the pharmacological correction of metabolic derangements in women with PCOS, no drug is currently recommended as a standard line of management. The apparent benefits of medical therapy must be weighed against the risk of potential adverse effects of prolonged treatment. Banaszewska B, Pawelczyk L, Spaczynski RZ, Dziura J, Duleba AJ. Effects of simvastatin and oral contraceptive agent on polycystic ovary syndrome: prospective, randomized, crossover trial. J Clin Endocrinol Metab 2007;92:456–61.
- 34. Surgical management Difficulty in sustaining lifestyle alterations and a lack of robust evidence supporting pharmacological interventions has spurred the search for newer modalities to manage metabolic syndrome in women with PCOS. Where other management strategies have failed, bariatric surgery may be offered to individuals with Class lll obesity (BMI ≥40 kg/ m2). Bariatric surgery may also be considered in women with Class II obesity (BMI 35–39.9 kg/m2) and associated chronic medical conditions such as diabetes and hypertension. Women undergoing bariatric surgery have demonstrated reduced cardiometabolic risk factors, reflected by an improved lipid profile and reduced insulin resistance. Common bariatric procedures include laparoscopic adjustable gastric banding, vertical banded gastroplasty and Roux-en-Y gastric bypass. Escobar-Morreale HF, Botella-Carretero JI, Alvarez-Blasco F, Sancho J, San Millan JL. The polycystic ovary syndrome associated with morbid obesity may resolve after weight loss induced by bariatric surgery. J Clin Endocrinol Metab 2005;90:6364–9. Gomez-Meade CA, Lopez-Mitnik G, Messiah SE, Arheart KL, Carrillo A, de la Cruz-Mu~noz N. Cardiometabolic health among gastric bypass surgery patients with polycystic ovarian syndrome. World J Diabetes 2013;4:64–9.
- 35. Surgical management These procedures have been found to be beneficial in reducing cardiovascular events, inducing remission of diabetes type II, hypertension, obstructive sleep apnoea and subsidence of metabolic syndrome. A metaanalysis of women with PCOS showed a significant reduction in the incidence of PCOS after bariatric surgery (from 45.6% to 6.8% at 12 months). Bariatric surgery may also reduce the incidence of obesity-related cancers. Although studies involving women with PCOS are limited, the results are encouraging. Further well-designed studies are required before bariatric surgery can form part of the mainstream management of metabolic syndrome in women with PCOS. Kwok CS, Pradhan A, Khan MA, Anderson SG, Keavney BD, Myint PK, et al. Bariatric surgery and its impact on cardiovascular disease and mortality: a systematic review and meta-analysis. Int J Cardiol 2014;173:20–8. Yu J, Zhou X, Li L, Li S, Tan J, Li Y, et al. The long-term effects of bariatric surgery for type 2 diabetes: systematic review and meta- analysis of randomized and non-randomized evidence. Obes Surg 2015;25:143–58. Skubleny D, Switzer NJ, Gill RS, Dykstra M, Shi X, Sagle MA, et al. The impact of bariatric surgery on polycystic ovary syndrome: a systematic review and meta-analysis. Obes Surg 2016;26:169–76.
- 36. Prevention is better than cure !! In order to prevent MetS, a multipronged approach is essential, which should include Behavior modification, Dietary modifications, Increase in physical activities, Prevention of smoking and alcohol excess. Prabhakaran D, Reddy KS. The metabolic syndrome: Looking beyond the debates. Clin Pharmacol Ther. 2011;90:19–21
- 37. School Schools offer an ideal medium for lifestyle interventions because the obesogenic lifestyle behaviors are less well developed in children and are therefore amenable to change. Bhatia V. IAP National Task Force for Childhood Prevention of Adult Diseases: Insulin resistance and type 2 diabetes mellitus in childhood. Indian Pediatr. 2004;41:443–57. Singhal N, Misra A, Shah P, Gulati S, Bhatt S, Sharma S, et al. Impact of intensive school-based nutrition education and lifestyle interventions on insulin resistance, β-cell function, disposition index, and subclinical inflammation among Asian Indian adolescents: A controlled intervention study. Metab Syndr Relat Disord. 2011;9:143–50
- 38. Prevention Target prepubertal and adolescent girl as they are the future mother’s Catch them young
- 40. Role of obstetrician OPD-adolescent PCOS and other adolescent pts Unique opportunity to counsel their mothers as well Community-school health programmes Pregnant lady-high index of suspicion from 1st visit-goal is to prevent not only in this pregnancy but in future pregnancies as well and also prevent MS in her later life (women’s dr)
- 41. Counselling Women diagnosed with PCOS should be informed of the possible long-term risks to health that are associated with their condition by their healthcare professional. Women should be made aware of the long-term implications of their condition, including their cardiovascular risk, by their healthcare professional, in a way that is tailored to their individual circumstances. Women should be made aware of the positive effect of lifestyle modification, including weight loss, for improving their symptoms, especially those who are overweight or obese. Women should be counselled that there is no strong evidence that PCOS by itself can cause weight gain or that having PCOS makes weight loss difficult or impossible.
- 42. Key take aways The risk factors for metabolic syndrome include central obesity,hypertension, atherogenic dyslipidaemia and insulin resistance. Metabolic syndrome affects 33% of women with polycystic ovary syndrome (PCOS) and has been less well researched than other features such as infertility, anovulation and hirsutism. Consequences of metabolic syndrome include cardiovascular disease, type II diabetes, cancer, sleep apnoea and psychological problems. Cardiometabolic risk screening involves obtaining data on smoking history, weight, body mass index, waist circumference, blood pressure, lipid profile, and taking an oral glucose tolerance test. Chandrasekaran S, Sagili H. Metabolic syndrome in women with polycystic ovary syndrome. The Obstetrician & Gynaecologist 2018;20:245–52. https://doi.org/10.1111/tog.12519
- 43. Key take aways Management of metabolic syndrome should focus on risk factors and individual components. Lifestyle modification is the only universally accepted intervention. Metformin may be considered in women with IGT, although there is no established duration of treatment. The use of newer drugs such as inositol and liraglutide require further validation, while the use of statins should be limited only to women with dyslipidaemia. Bariatric surgery can be considered as a last resort in appropriately selected women. Prevention is better than cure-Catch them young in schools and OPD
- 44. My World of sharing happiness! Shrikhande Fertility Clinic Ph- 91 8805577600 shrikhandedrlaxmi@gmail.com
- 45. Questions
- 46. The Art of Living Anything that helps you to become unconditionally happy and loving is what is called spirituality. H. H. Sri Sri Ravishakar
Editor's Notes
- Diagnosis of metabolic syndrome.Key: NCEP:ATP III = National Cholesterol Education Program Adult Treatment Panel III; AHA/NHLBI = the American Heart Association/National Heart, Lung, and Blood Institute; IDF = International Diabetes Federation; JIS = Joint Interim Statement. IF THIS IMAGE HAS BEEN PROVIDED BY OR IS OWNED BY A THIRD PARTY, AS INDICATED IN THE CAPTION LINE, THEN FURTHER PERMISSION MAY BE NEEDED BEFORE ANY FURTHER USE. PLEASE CONTACT WILEY'S PERMISSIONS DEPARTMENT ON PERMISSIONS@WILEY.COM OR USE THE RIGHTSLINK SERVICE BY CLICKING ON THE 'REQUEST PERMISSIONS' LINK ACCOMPANYING THIS ARTICLE. WILEY OR AUTHOR OWNED IMAGES MAY BE USED FOR NON-COMMERCIAL PURPOSES, SUBJECT TO PROPER CITATION OF THE ARTICLE, AUTHOR, AND PUBLISHER.
- Components of a healthy diet for women with polycystic ovary syndrome. IF THIS IMAGE HAS BEEN PROVIDED BY OR IS OWNED BY A THIRD PARTY, AS INDICATED IN THE CAPTION LINE, THEN FURTHER PERMISSION MAY BE NEEDED BEFORE ANY FURTHER USE. PLEASE CONTACT WILEY'S PERMISSIONS DEPARTMENT ON PERMISSIONS@WILEY.COM OR USE THE RIGHTSLINK SERVICE BY CLICKING ON THE 'REQUEST PERMISSIONS' LINK ACCOMPANYING THIS ARTICLE. WILEY OR AUTHOR OWNED IMAGES MAY BE USED FOR NON-COMMERCIAL PURPOSES, SUBJECT TO PROPER CITATION OF THE ARTICLE, AUTHOR, AND PUBLISHER.
- Combating the metabolic syndrome— either as it is commonly understood or through the various components of the syndrome at the population level— is complex and requires multisectoral policy approaches. Policy changes should focus on providing balanced nutrition and an enabling environment for improving physical activity. For physicians treating individuals at high risk, aggressive lifestyle modification will remain the mainstay, until such individuals reach thresholds for drug therapy.[111]
- Schools offer an ideal medium for lifestyle interventions because the obesogenic lifestyle behaviors are less well developed in children and are therefore amenable to change.[102] Moreover, it is important to identify the adolescents at risk for T2DM and CHD at an early age and use appropriate prevention strategies while the pathological processes are still reversible.[103,104]
