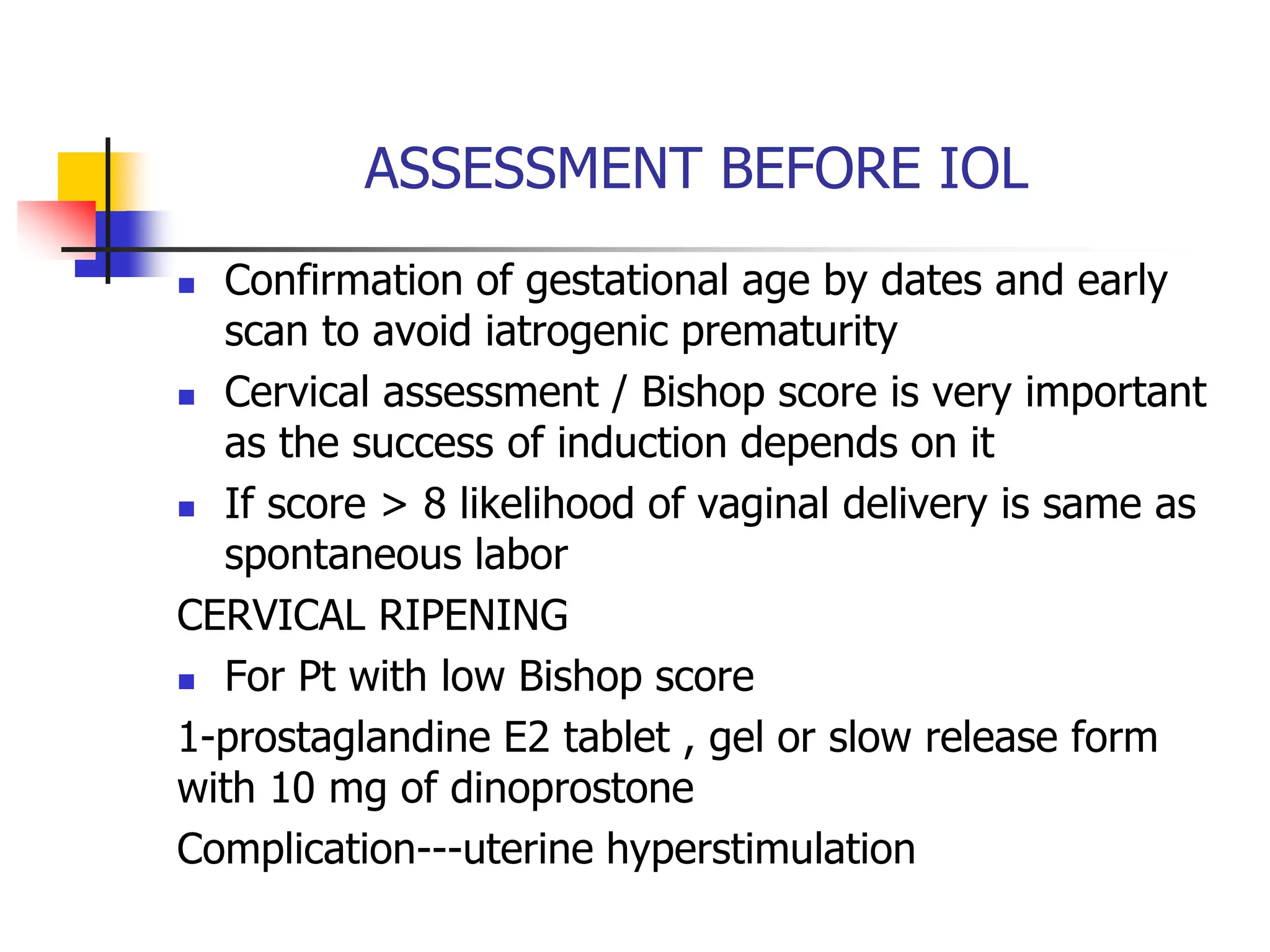
The document discusses post-term pregnancy, defined as a pregnancy extending beyond 294 days, with an incidence of 7-11%. It covers diagnosis, complications, and management including induction of labor, emphasizing the importance of fetal monitoring and criteria for induction. The document also outlines indications and contraindications for induction, methods used, and the associated risks and complications.