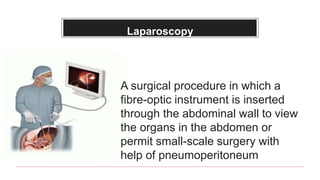
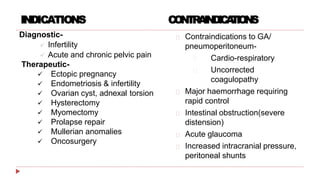
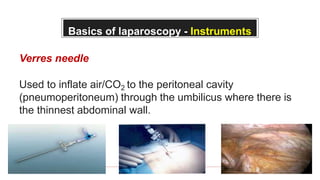
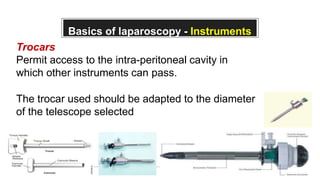
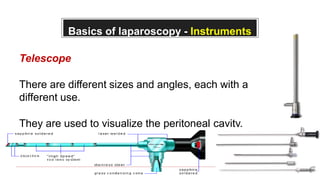
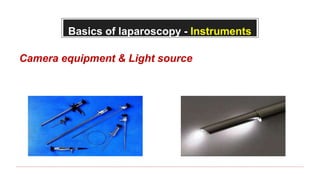
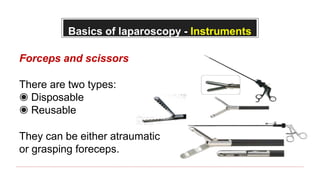
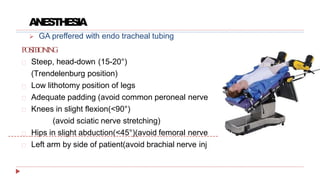
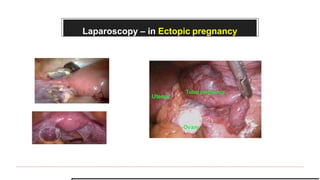
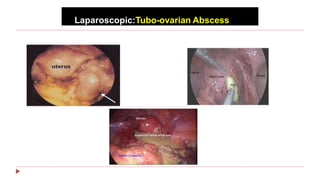
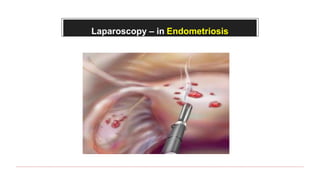
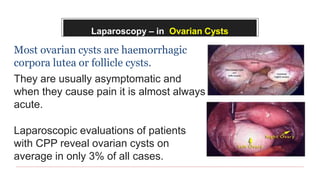
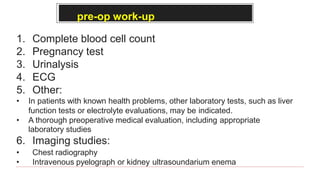
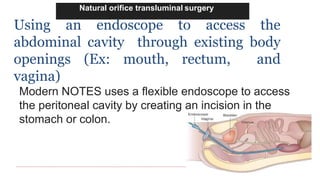
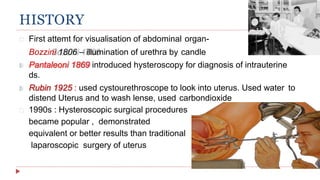
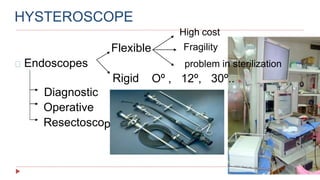
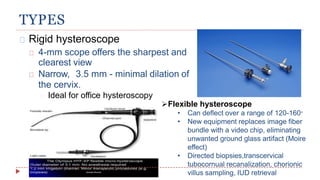
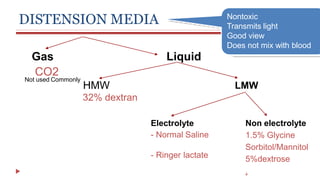
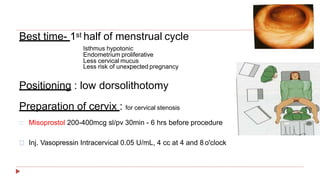
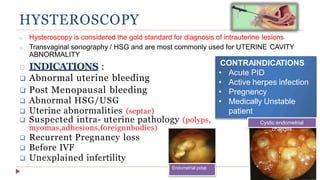
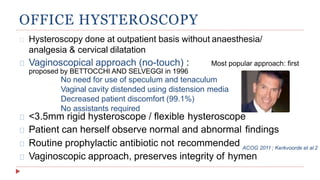
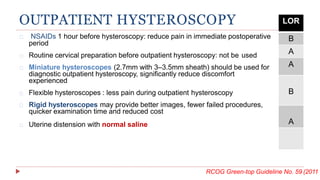
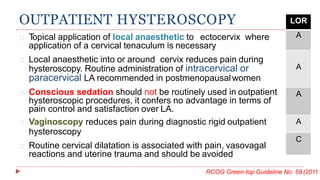
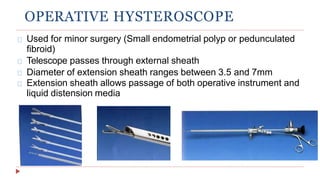
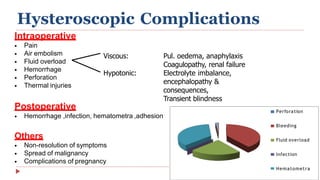
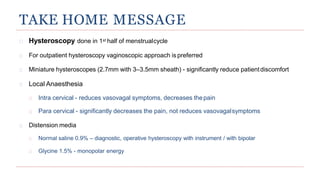
This document provides information about laparoscopy and hysteroscopy procedures. It begins with the basics of laparoscopy, including a definition, brief history, and descriptions of the instruments used. Advantages include reduced postoperative pain and recovery time compared to open surgery. Risks include potential injuries. Hysteroscopy allows direct visualization of the uterine cavity using a small telescope inserted through the cervix. Various devices and distension media options are described. Common indications for both procedures include diagnostic evaluation and treatment of conditions like endometriosis, cysts, and fibroids. Overall the document outlines the key elements of minimally invasive laparoscopic and hysteroscopic surgeries.