This document provides an overview of key laboratory safety topics, including:
- The hierarchy of controls for hazards and types of engineering, administrative and personal protective controls.
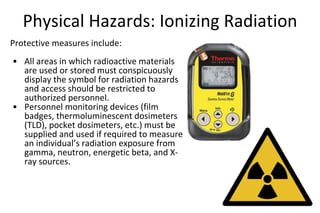
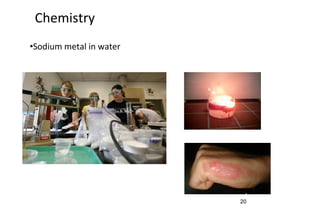
- Chemical, biological and physical hazards like noise, radiation and ergonomics. It outlines exposure limits and safety measures.
- Requirements for chemical hygiene plans, exposure monitoring, medical exams, hazard communication, and more.
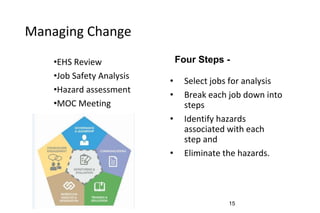
- Best practices for working with research animals, managing change, conducting safety training, and chemical inventory control.
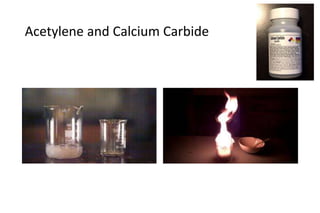
- Examples of incidents involving water-reactive chemicals and lack of proper protective equipment emphasize importance of compliance.