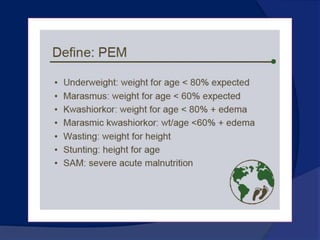
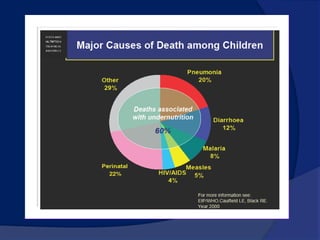
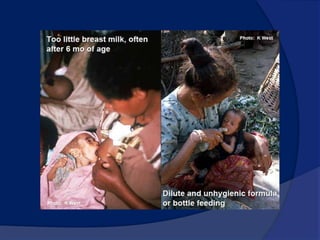
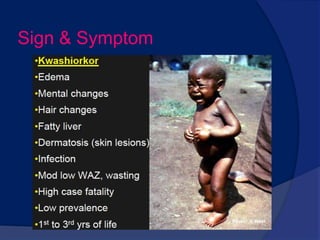
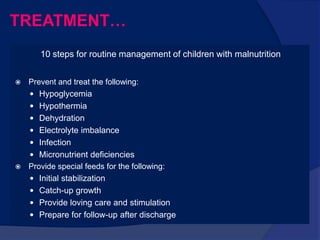
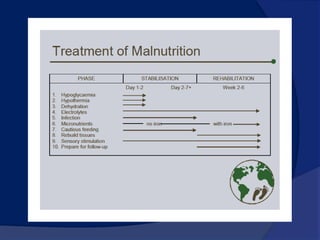
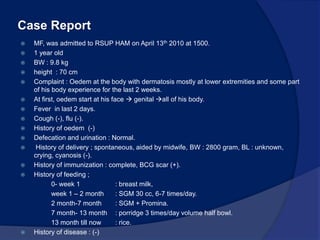
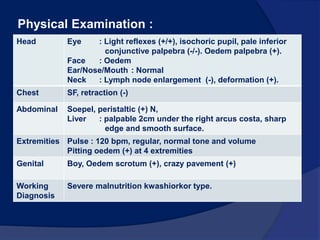
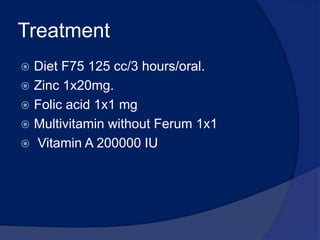
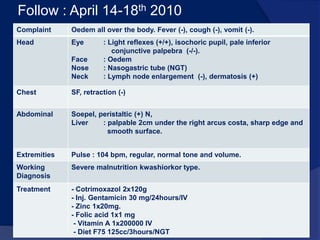
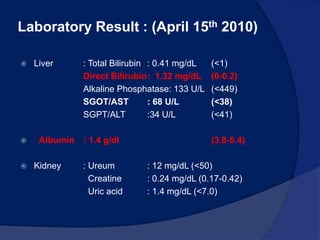
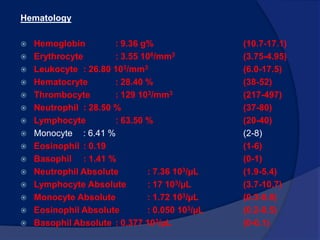
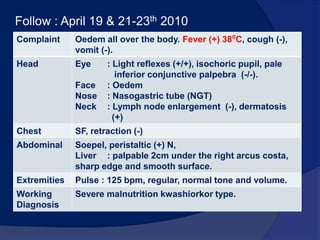
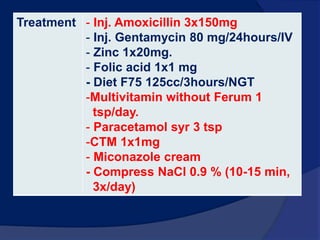
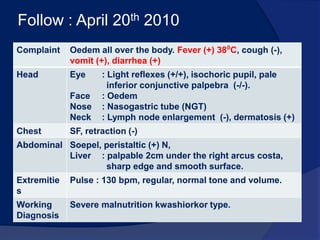
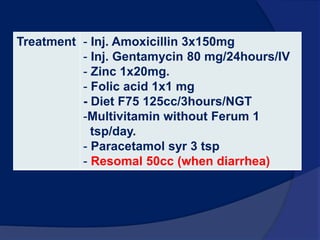
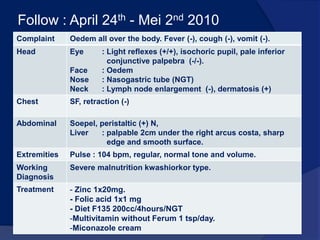
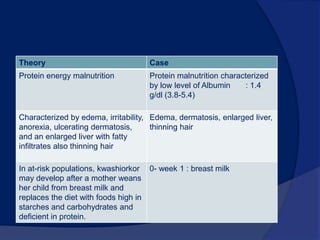
The document discusses Kwashiorkor, a type of severe protein-calorie malnutrition. It defines Kwashiorkor and provides details on its epidemiology, causes, signs and symptoms, and pathophysiology. The document also presents a case report of a 1-year old boy admitted with edema all over his body who was diagnosed with severe kwashiorkor. His treatment and progress over 2 weeks in the hospital are described.