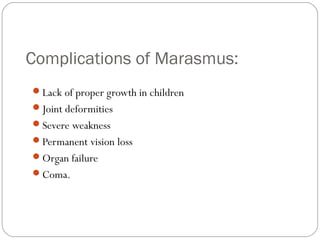
Marasmus is a form of severe protein-energy malnutrition that occurs due to negative energy balance, particularly in infants. It is characterized by severe wasting of over 60% of expected weight, loss of subcutaneous fat and muscle wasting. The causes include poor feeding habits, physical defects preventing eating, diseases interfering with food assimilation, infections causing loss of appetite, and loss of food through vomiting or diarrhea. Treatment involves rehydration and refeeding through intravenous fluids or feeding tubes to prevent complications like organ failure or coma from developing.