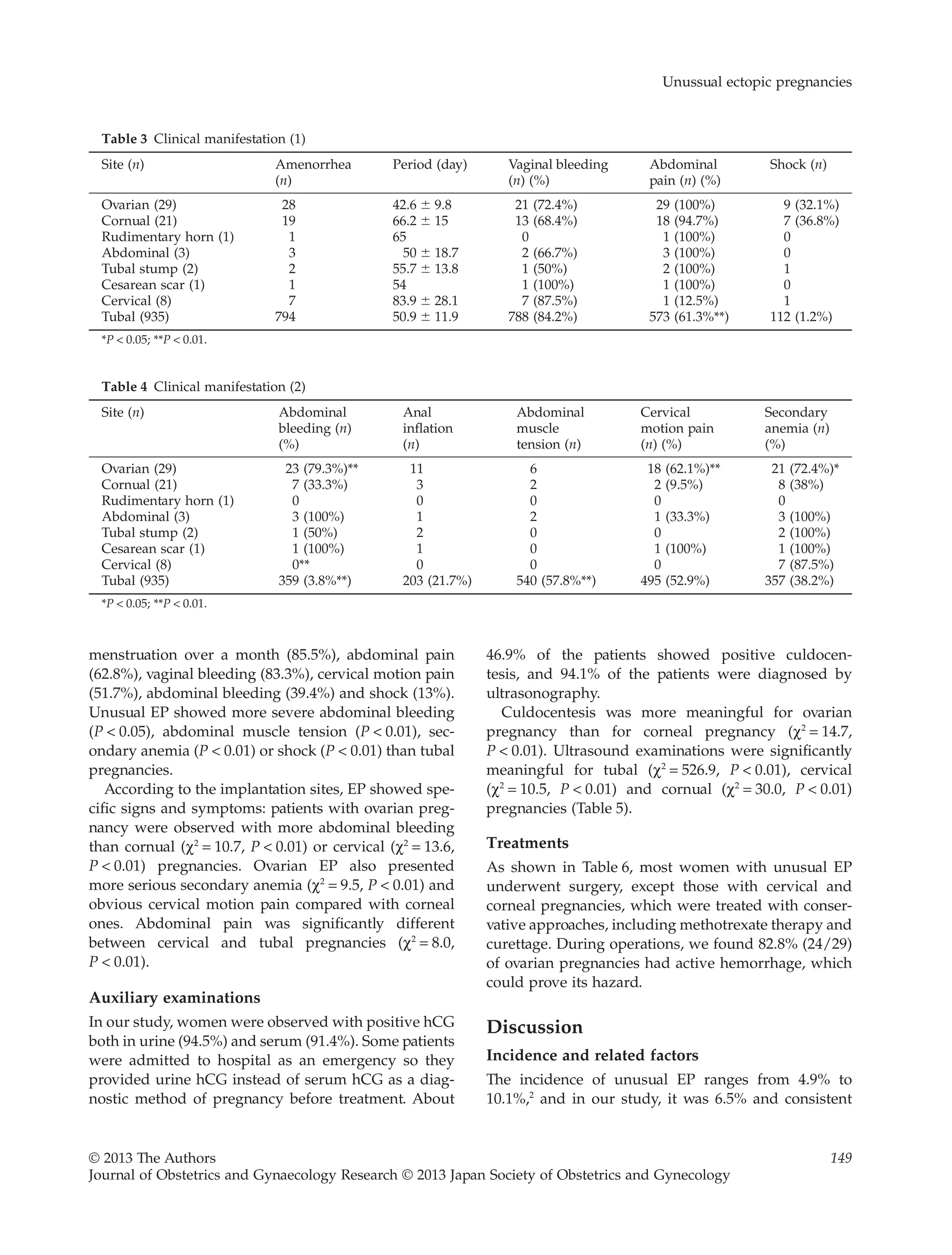
This study retrospectively analyzed 65 cases of unusual ectopic pregnancies out of 1000 total ectopic pregnancy cases over a 10-year period. The study found that ovarian pregnancies were associated with intrauterine device placement and pelvic inflammatory diseases. Extratubal ectopic pregnancies like those in the ovaries, cervix, and abdomen presented more serious symptoms and had higher misdiagnosis rates than tubal pregnancies. Most unusual ectopic pregnancies required surgery for treatment, though some early cervical and corneal pregnancies were treated with conservative methods like mifepristone and methotrexate or curettage.

![with the reports. Although this incidence is low, the
danger and mobility from an extratubal pregnancy is
higher than normal pregnancy. Moreover, the success
rate for a subsequent pregnancy will be reduced after
EP.
In our series, the most common site of implantation
in EP is the tube, followed by the ovary, corn, cervix
and abdomen. The rarest site is the cesarean scar.
Ovarian pregnancy is very rare, accounting for 0.3%–
3.0% of EP,3
and its incidence in our investigation was
3.1%. Ovarian pregnancy is generally believed to be
associated with pelvic inflammatory diseases and pre-
vious surgery in the pelvic cavity. We found 44.8% of
the cases (13/29) had a history of pelvic inflammatory
diseases, and 55.2% (16/29) had a history of delivery or
curettage. Patients with a history of pelvic inflamma-
tory diseases showed a significant difference in ovarian
than corneal and tubal pregnancies. Furthermore, even
without inflammatory history, pelvic surgeries may
also cause ovarian inflammation and thicken the albug-
inea, which could lead to a relative lack of follicular
fluid pressure. Finally, it would generate ovulation dis-
order. Ovum might be detained in the broken follicles
and fertilized just in the ovary.
Reportedly, the use of IUD seems to be dispropor-
tionately associated with ovarian pregnancy.4,5
In our
series, 10 out of 29 patients had a history of IUD place-
ment (27.6%), which indicated statistical relevance
between IUD and ovarian pregnancy, and suggested
that IUD placement may change some manners in the
pathophysiological environment of the ovary. IUD was
hypothesized to successfully prevent all pregnancies,
except ovarian ones.6
Therefore, the history of IUD
placement is useful if a patient is suspected of ovarian
pregnancy. However, it was reported that the incidence
rate of PID among IUD users as reported from different
studies depends heavily on the definition used and the
means available for diagnosing PID. It varies from 1 per
100 to 1 per 1000 woman-years – a tenfold difference –
in different studies. PID risk has been found to be
sixfold higher in the first month after IUD insertion
than it is thereafter. Beyond the first month or so after
insertion, the incidence of PID is low among women
using IUD and at a level that appears similar to that for
women in general.7
The incidence of cervical pregnancy is less than 1%
of all EP,8,9
varying from 1/10003
to 1/18 000.4
the cause
may be associated with the following factors: (i) cesar-
ean section and usage of IUD might interfere with the
implantation of blastocyst; (ii) repeated endometrial
curettages might damage the endometrium or form a
scar, and thus retard the pass and implantation of blas-
tocyst at cervix (in our series, 75% of the cases [6/8]
reported a history of induced abortion or cesarean
section and placement of IUD, which suggested that
intrauterine surgeries could be an important cause for
cervical pregnancy); and (iii) with the development of
reproductive technology, embryo transfer as in vitro
fertilization is also a substantial cause.
Misdiagnosis rate
The misdiagnosis rate of extratubal pregnancies is
quite high (96.6%). Ovarian and tubal pregnancies are
difficult to distinguish, even by ultrasound, because
their clinical manifestations are similar. In our investi-
gation, only one case of ovarian pregnancy was diag-
nosed by ultrasound. Reportedly, all 24 cases of ovarian
pregnancies in six hospitals were preoperatively mis-
diagnosed.10
However, positive culdocentesis results
were more common in patients with ovarian pregnan-
cies than with cornual pregnancies, probably because a
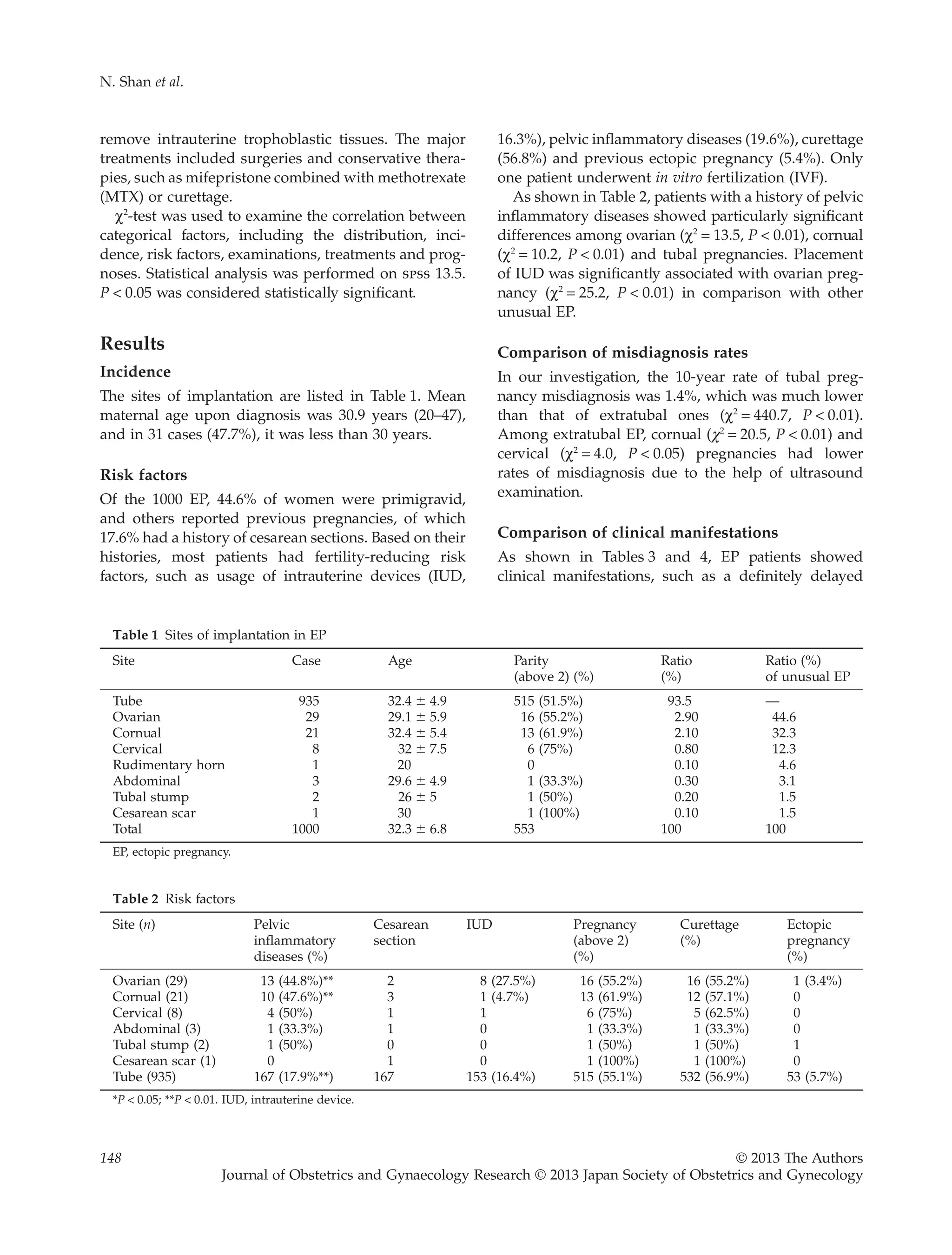
Table 5 Auxiliary examination
Site (n) Serum
hCG (n)
Urine
hCG (n)
Culdocentesis
positive
(n)
Ultrasound
Diagnosis
(n)
fetal heart
movement
Persistent
hCG
secretion
Cases of
misdiagnosis
Ovarian (29) 17 (58.6%) 25 (86.2%) 20** (69%) 1 (3.4%) 1 (3.45%) 6 (20.7%) 28 (96.6%**)
Cornual (21) 13 (61.9%) 13 (61.9%) 3 (14.3%) 12 (57.1%) 0 0 5 (23.8%**)
Cervical (8) 6 (75%) 5 (62.5%) 0 5 (62.5%) 0 0 2 (25%*)
Rudimentary horn (1) 1 (100%) 1 (100%) 0 1 (100%) 0 1 (100%) 0
Abdominal (3) 2 (66.7%) 2 (66.7%) 0 0 2 (66.7%) 0 3 (100%)
Tubal stump (2) 0 2 (100%) 1 (50%) 0 0 0 2 (100%)
Cesarean scar (1) 1 (100%) 1 (100%) 0 0 0 0 1 (100%)
Tubal (935) 874 (93.5%) 896 (95.8%) 445 (47.6%) 922 (98.6%) 38 (4.06%) 0 13 (1.4%**)
Total 914 (91.4%) 945 (94.5%) 46.9 (46.9%) 941 (94.1%) 41 (4.1%) 7 (0.7%) 54 (5.4%)
*P < 0.05; **P < 0.01. hCG, human chorionic gonadotrophin.
N. Shan et al.
150 © 2013 The Authors
Journal of Obstetrics and Gynaecology Research © 2013 Japan Society of Obstetrics and Gynecology](https://image.slidesharecdn.com/unusualectopicpregnancies-140317061353-phpapp02/75/Unusual-ectopic-pregnancies-4-2048.jpg)
![implanted in the cervical canal, the higher capacity it
has to grow and hemorrhage. Some diagnostic criteria
for cervical pregnancy are:
1 Clinical signs and symptoms: recurring vaginal
bleeding without pain was observed during early
gestation, often followed by uncontrolled hemor-
rhage. In our investigation, 87.5% (7/8) of cases were
observed with vaginal bleeding, involving three
cases of emergency.
2 Gynecological examination: cervix is dilated; cervical
canal increasingly thickens like barrel. Doctors could
see or even touch placenta in cervix. Two cases pre-
sented cervical dilation and another two cases
showed a flabby cervix. The examination may cause
severe hemorrhage, so it should be deliberated
before examination.
3 Serum b-hCG assessment and ultrasound examina-
tion. Quantitative serum hCG in cervical pregnancy
is often present below the normal pregnancy due to
poor blood supply. Compared with other unusual
EP, cervical pregnancy showed atypical abdominal
pain or bleeding. This may be the result of early
admission.
In abdominal pregnancy, with either tubal abortion or
intraperitoneal rupture, the entire conceptus may
be extruded from the tube. If an early conceptus is
expelled essentially undamaged into the peritoneal
cavity, its placental attachment may persist, or it may be
reimplanted almost anywhere and grow as an abdomi-
nal pregnancy. This is unusual, and most small concep-
tuses can be reabsorbed. They may occasionally remain
in the cul-de-sac for years as an encapsulated mass, or
even become calcified to form a lithopedion.11
All our cases are secondary. The first one occurred
due to rupture of tubal pregnancy, and then the con-
ceptus developed on the posterior wall of bladder. The
second one was from rupture of rudimentary horn
pregnancy and the conceptus grew in Douglas’ space
on the ligament of the right iliac fossa. The last one
happened due to tubal interstitial pregnancy and the
conceptus dropped into the abdominal cavity. During
the operation, the fetus was found alive in the abdomi-
nal cavity surrounded by blood. The placenta was
attached to the greater omentum.
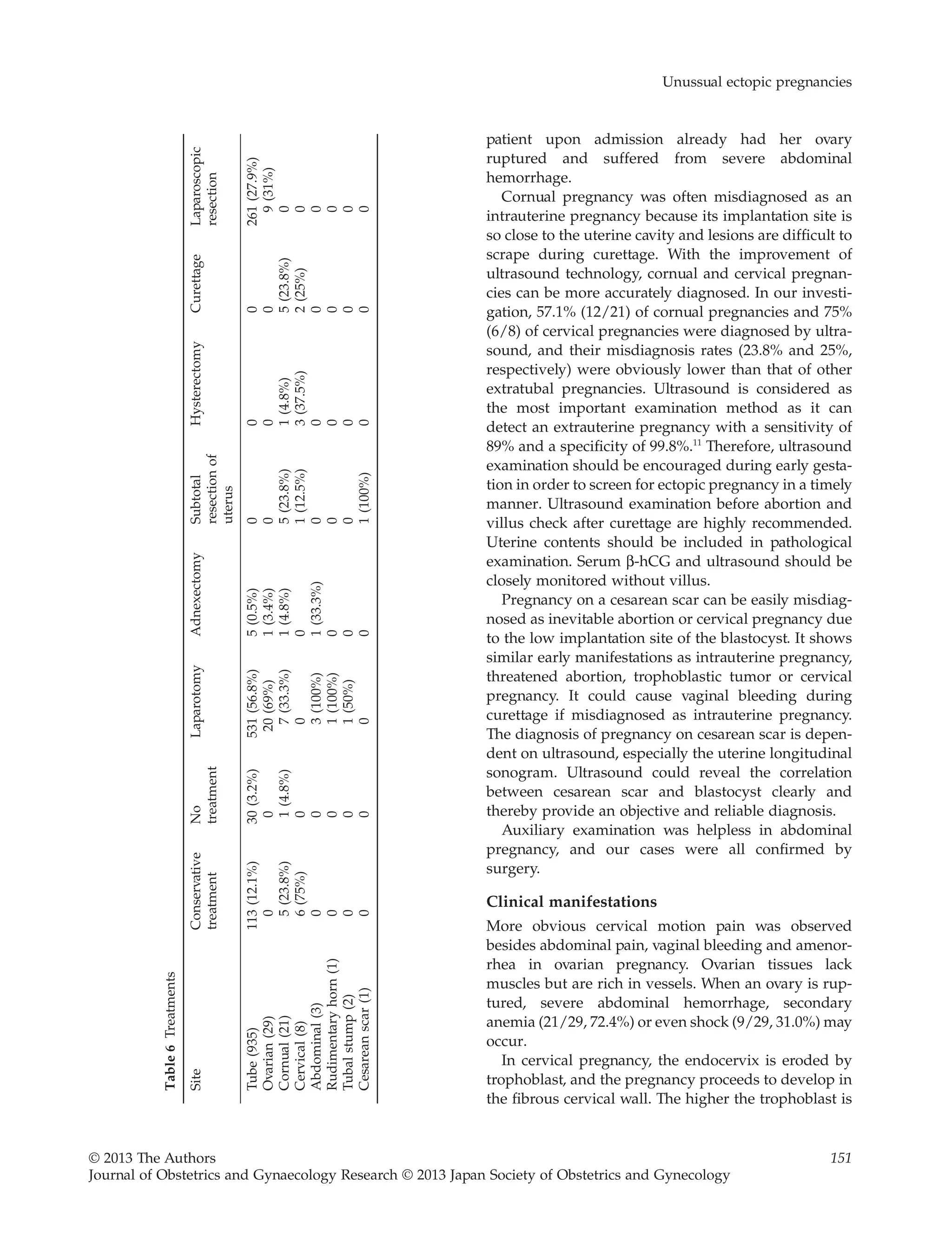
Treatment and prognosis
Twenty-eight out of 29 women with ovarian preg-
nancies underwent surgery by resection of the ovarian
wedge or partial oophorectomy. Most reports advocate
preserving ovarian tissues as much as possible.
Doctors cut off the affected annex only under serious
damages.
In the past, it was suggested to cut off the uterine
corpus to avoid rupture of cornual pregnancy, and
hysterectomy was recommended if necessary. In our
study, seven cases (33.3%) underwent lesion resection
on corpus; and five cases (23.8%) received sub-
total hysterectomy due to ruptures. In recent years,
many successful cases of conservative treatment were
reported. We treated five patients with conservative
therapies, including mifepristone, curettage and
MTX, which achieved excellent results. However,
some reports also pointed out that conservative treat-
ment for patients in this type of pregnancy with long-
time amenorrhea and abdominal pain may not
succeed easily.
Before 12 weeks’ gestation, invasion of trophoblastic
cells in the cervical wall is not deep enough, so conser-
vative treatments for cervical pregnancy can be suc-
cessful.12
Treatments include: (i) hysterectomy and
subtotal hysterectomy (they are operated only after
failure of conservative treatments or uncontrolled hem-
orrhage [they were used in three cases]); and (ii) con-
servative treatments (the key was early diagnosis and
treatment). Recently, the use of curettage and hysterec-
tomy has been reduced gradually. They are only used
as alternative therapies for MTX and uterine artery
embolization. Reportedly, MTX can be used by sys-
temic or local injection. It could reach a high effect of
80%.13
Usage of both mifepristone and MTX was better
than single MTX for cervical pregnancy, as the former
showed a high success rate and lower toxicity.14
This
method could enhance the toxicity to trophoblast cells
and kill the embryo effectively.
In our investigation, four cases of conservative treat-
ments and two cases of curettage were successful.
However, vaginal bleeding may still occur after con-
servative treatments. Doctors should closely monitor
patients’ conditions. One patient underwent hysterec-
tomy after conservative treatment due to recurring
vaginal bleeding.
Rudimentary horn in the uterus is the result of devel-
opmental defects on lower segment in the duct of
Muller, which caused unequal formation on both sides.
A small appendage formed next to the normal uterus
and connected it through a bunch of fibrous tissues.15
Compared with the normal uterus, the rudimentary
uterus has thicker muscles (most hypoplasia) with
dense vessels. Thus, severe hemorrhage often occurs
after the rupture of pregnancy.
N. Shan et al.
152 © 2013 The Authors
Journal of Obstetrics and Gynaecology Research © 2013 Japan Society of Obstetrics and Gynecology](https://image.slidesharecdn.com/unusualectopicpregnancies-140317061353-phpapp02/75/Unusual-ectopic-pregnancies-6-2048.jpg)

