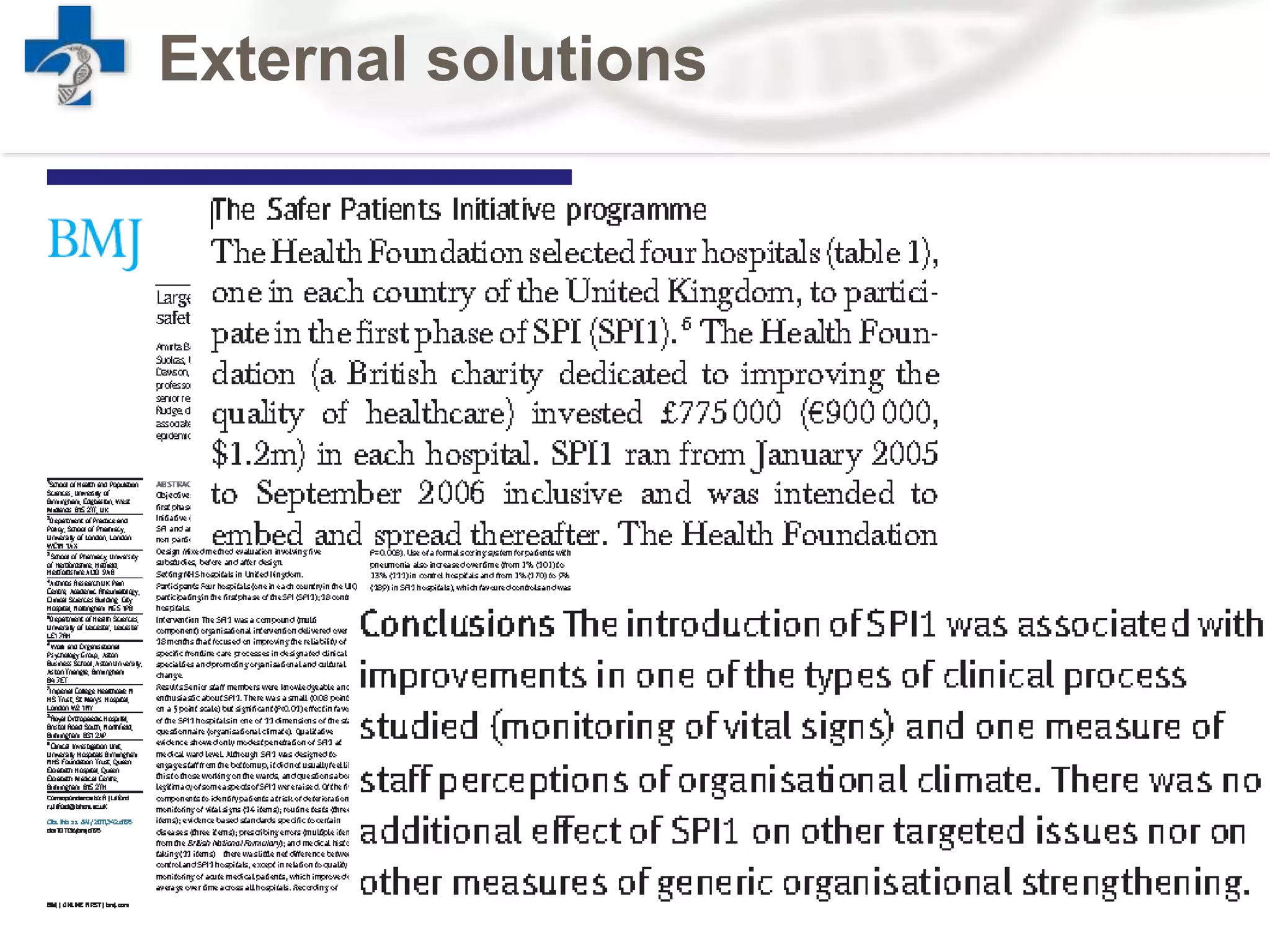
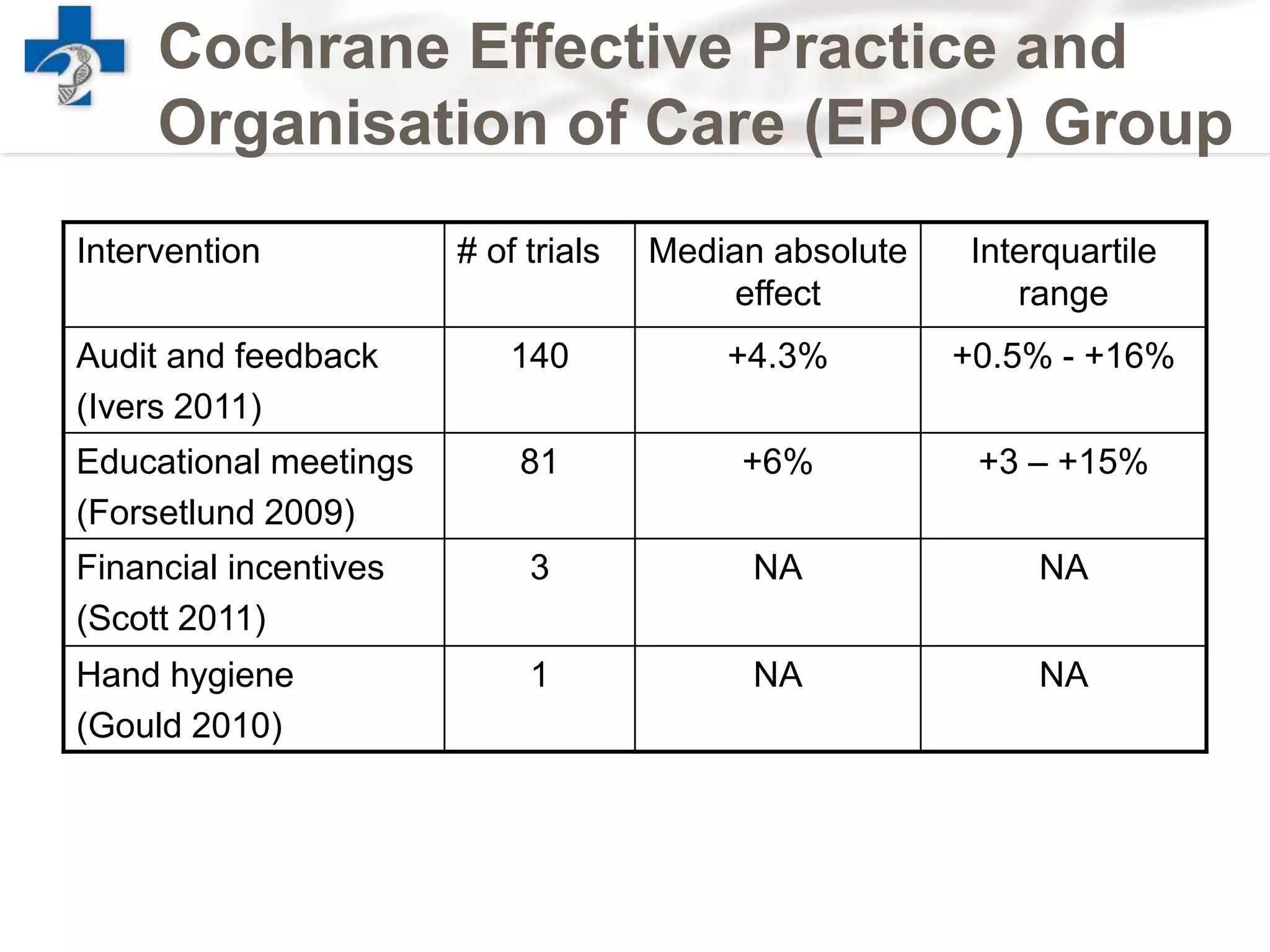
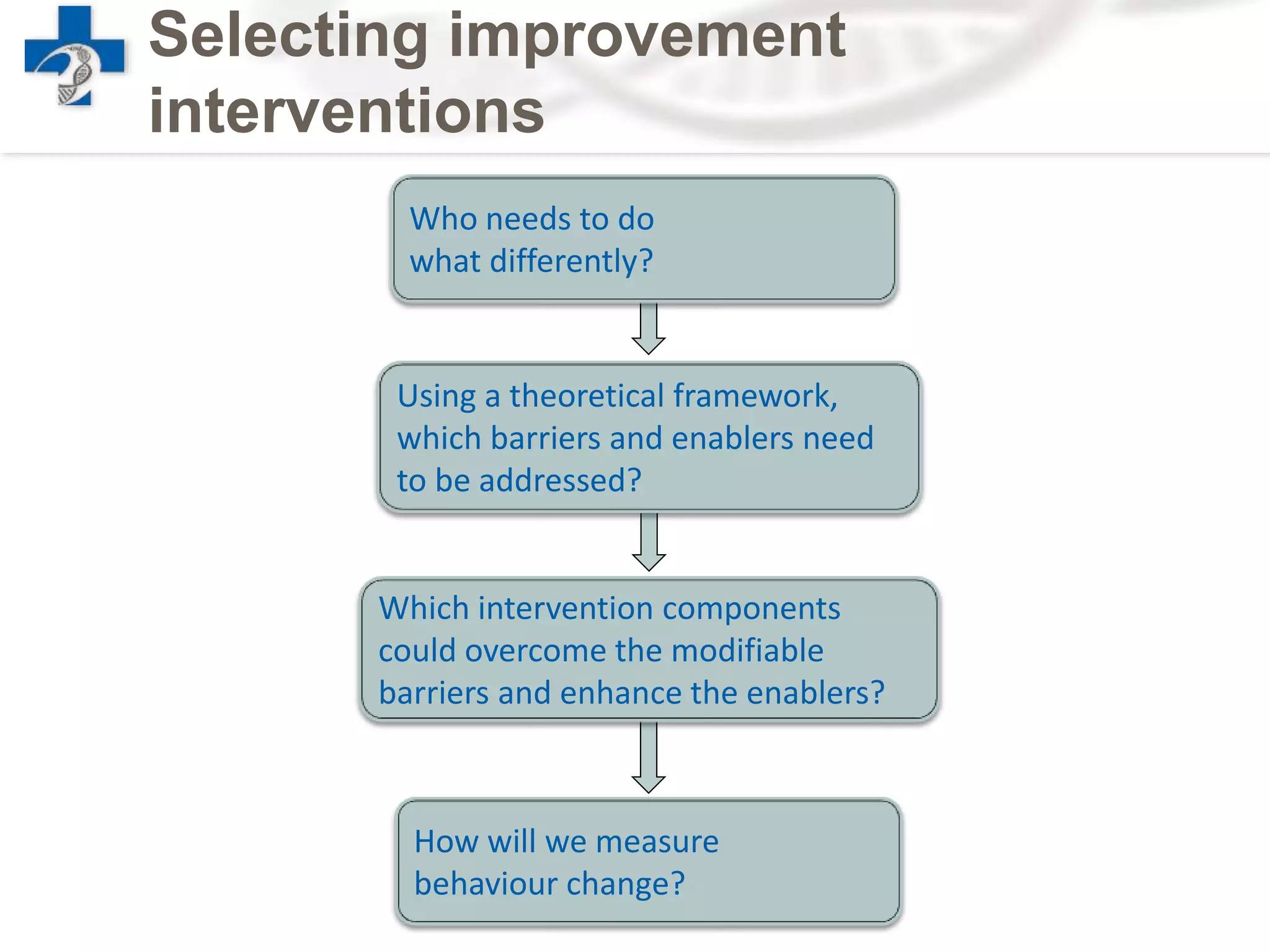
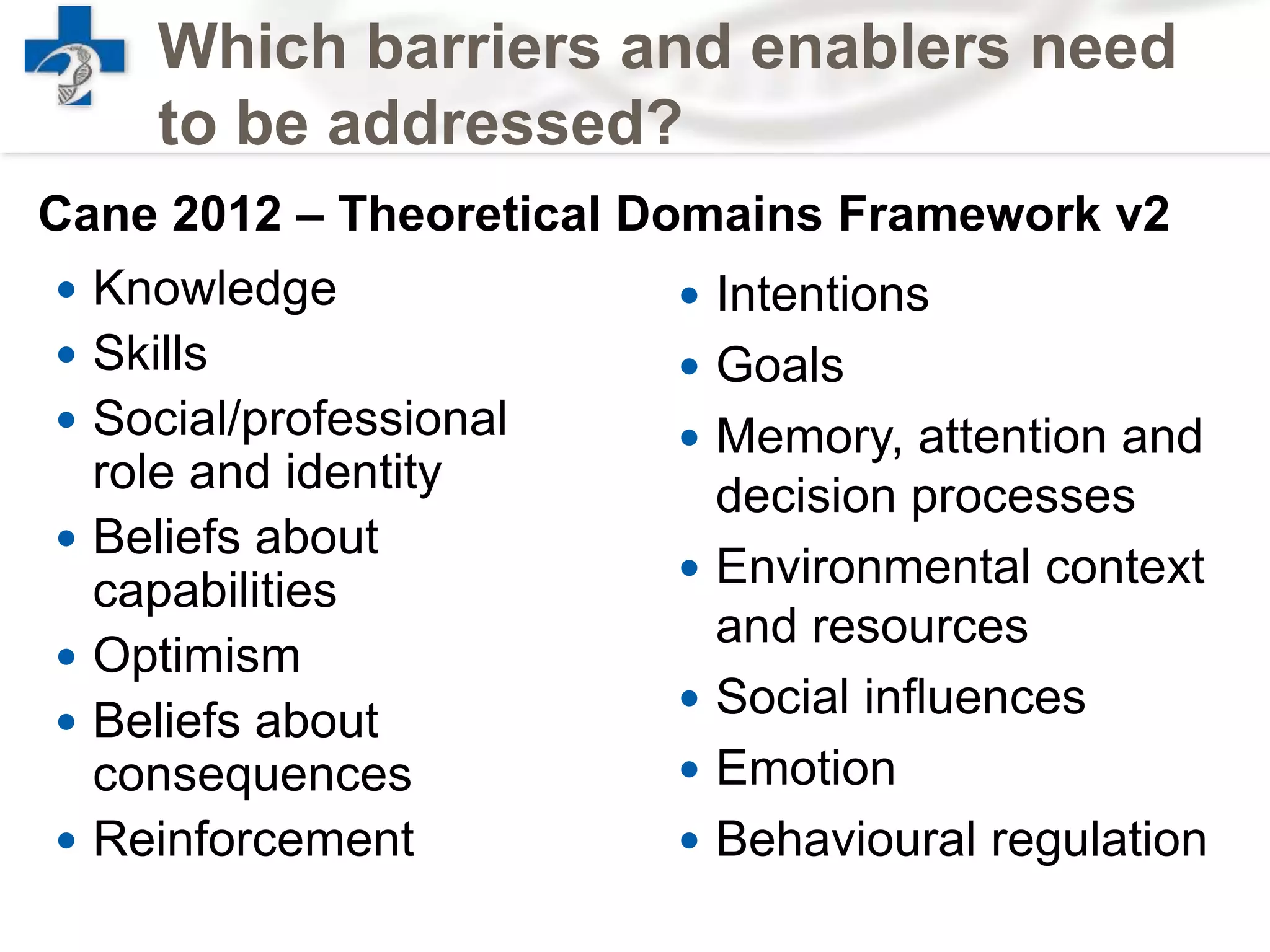
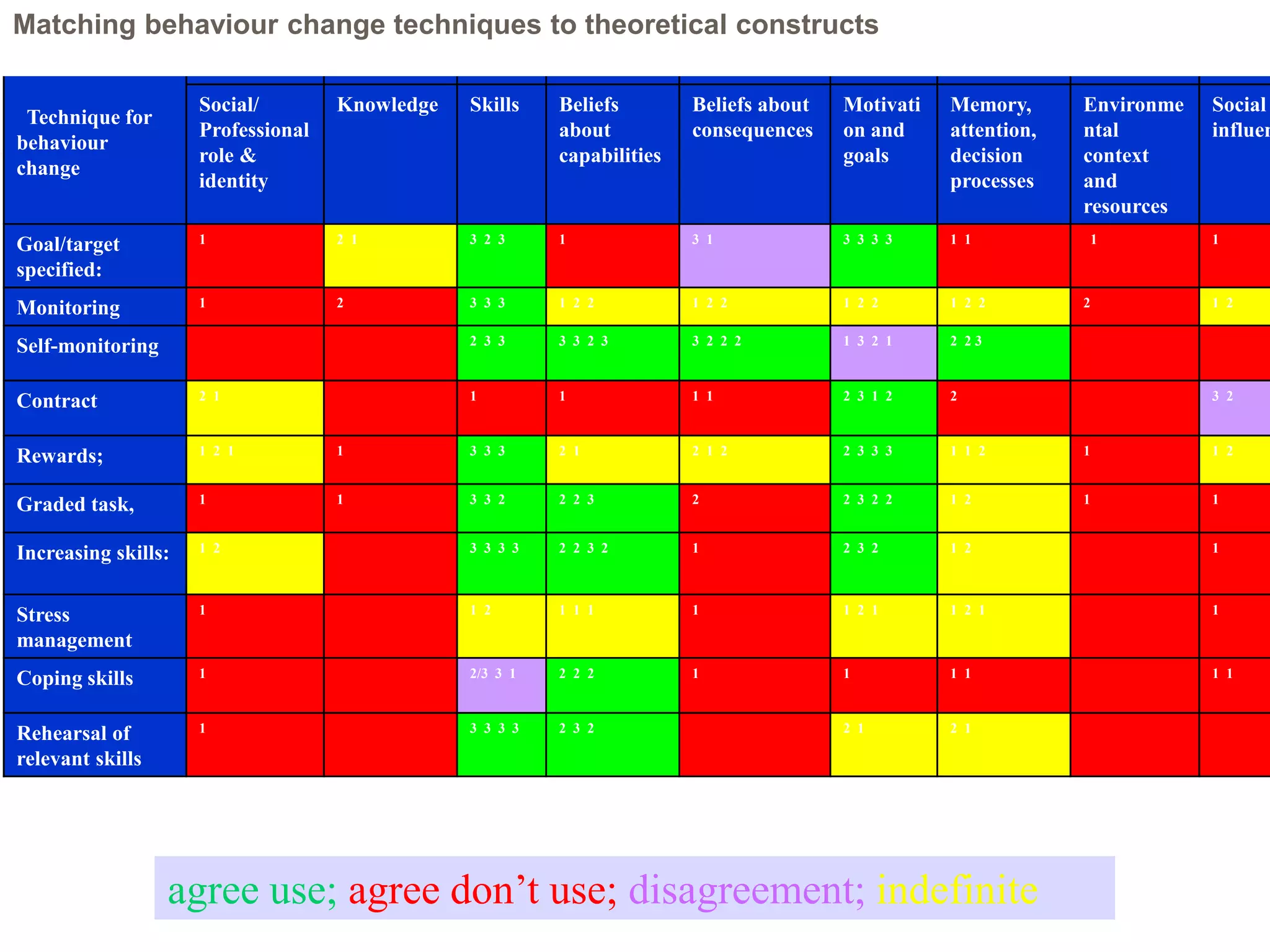
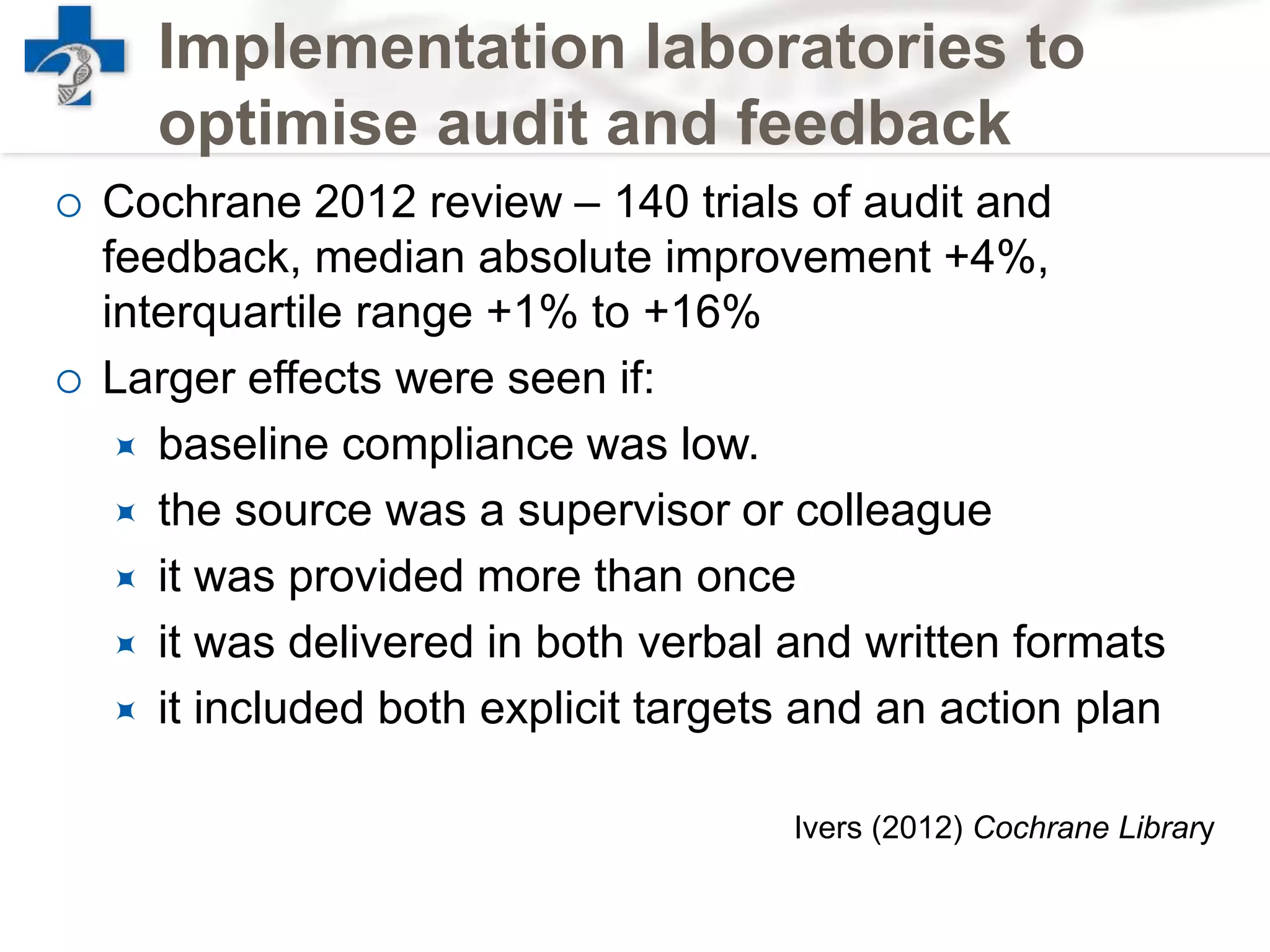
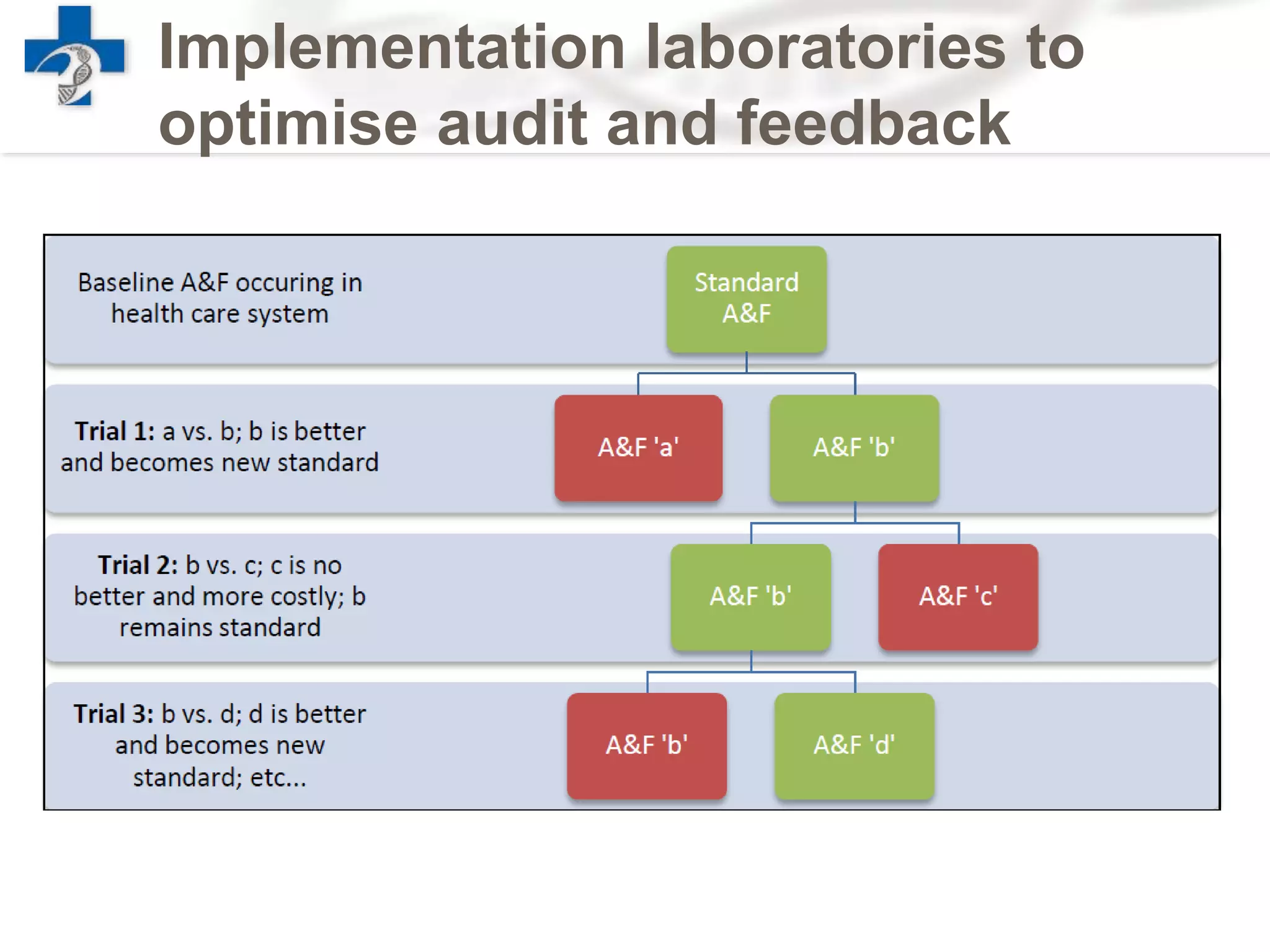
The document discusses the challenges of improving clinical services in healthcare, highlighting the gap between research findings and clinical practice where a significant proportion of patients either receive ineffective treatment or unnecessary care. It emphasizes the need for evidence-based implementation alongside evidence-based medicine to determine which interventions are most effective and efficient in improving healthcare outcomes. The author proposes a systematic approach to understanding behavior change in healthcare as a means to optimize clinical service improvements.