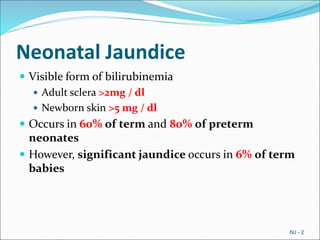
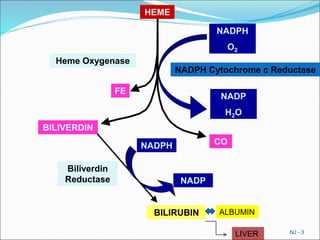
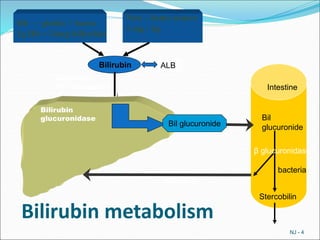
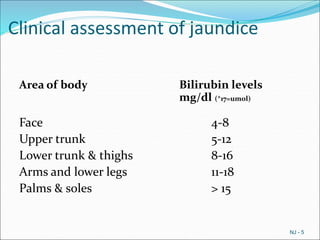
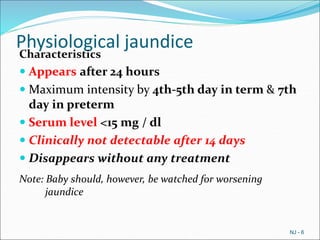
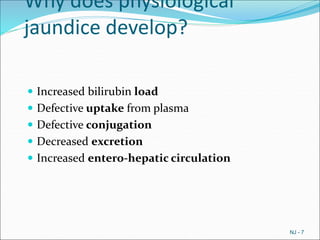
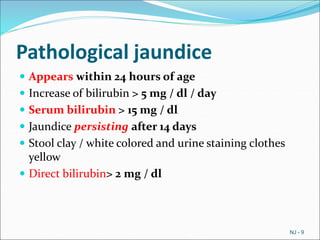
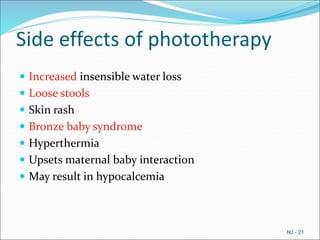
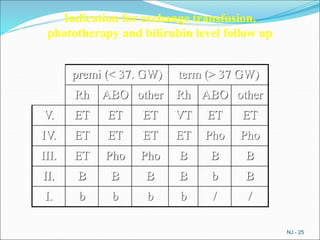
Neonatal jaundice occurs in 60% of term and 80% of preterm neonates. It is caused by an imbalance between bilirubin production and excretion in newborns. Jaundice is classified as either physiological or pathological based on timing of onset, bilirubin levels, and duration. The document discusses the mechanisms, risk factors, clinical assessment, investigations, management including phototherapy and exchange transfusion, and various causes of neonatal jaundice.