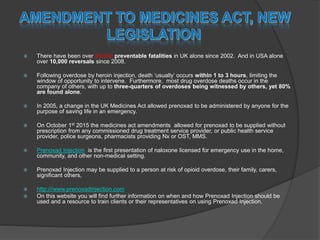
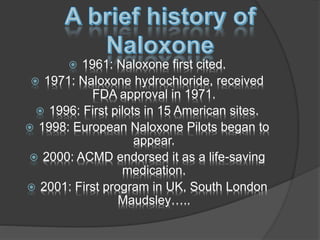
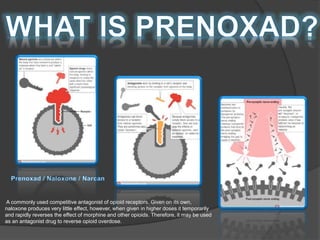
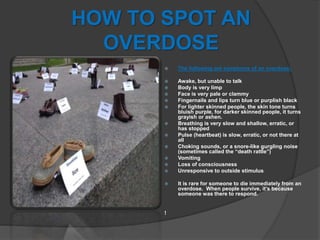
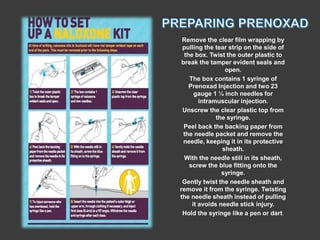
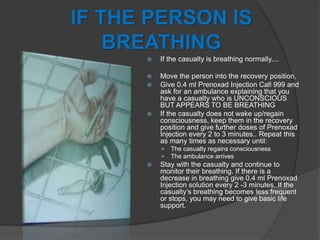
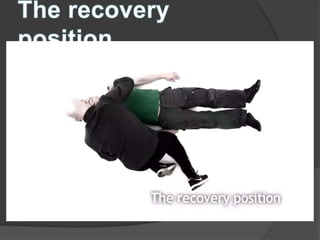
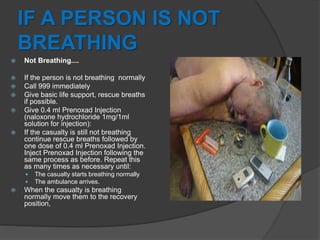
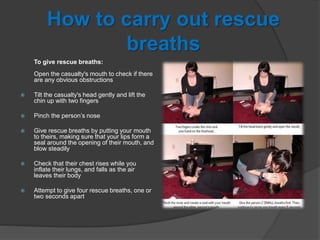
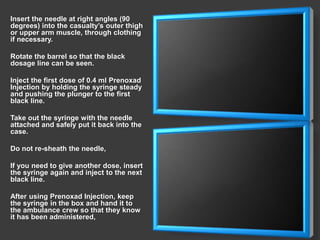
The document discusses the critical issue of opioid overdose fatalities, with over 28,000 preventable deaths in the UK since 2002 and 10,000 reversals in the USA since 2008, highlighting the importance of immediate intervention. It details the legal changes allowing the emergency administration of the naloxone formulation 'prenoxad', which can be supplied without a prescription to individuals at risk and their support networks. The document also provides guidelines on recognizing overdose symptoms and administering prenoxad effectively to save lives.