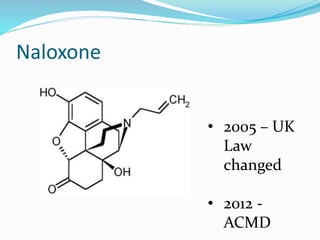
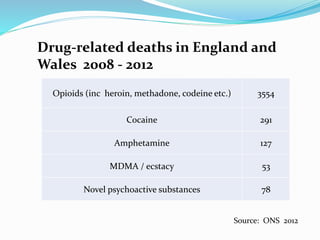
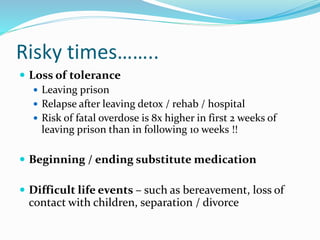
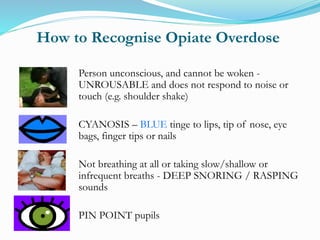
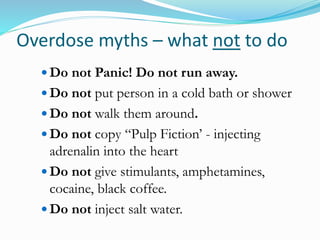
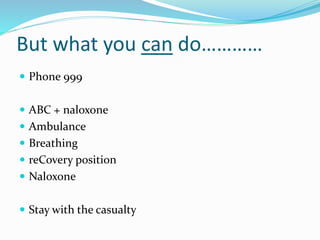
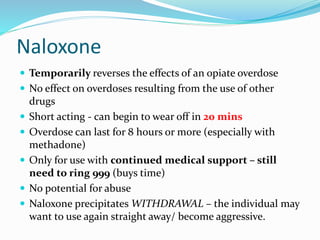
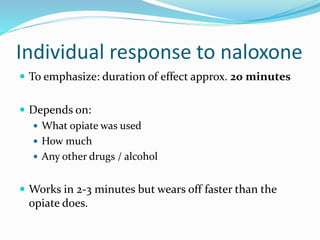
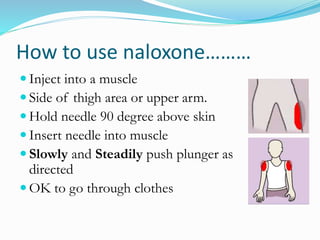
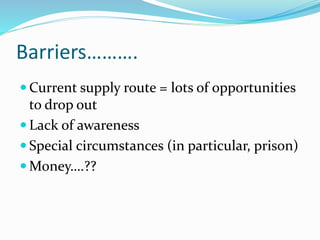
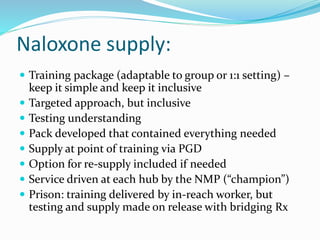
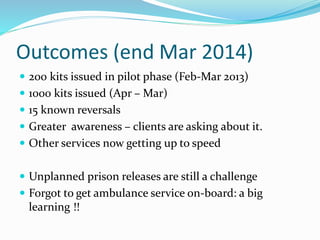
This document discusses opioid overdose and the use of naloxone to reverse overdoses. It provides statistics on drug-related deaths in the UK and risk factors for overdose. Naloxone is described as a temporary antidote that reverses the effects of opioid overdose by binding to opioid receptors but not activating them. The document outlines how to recognize an overdose, administer naloxone via injection, and the need to still call emergency services. Barriers to naloxone access and potential future developments are mentioned.