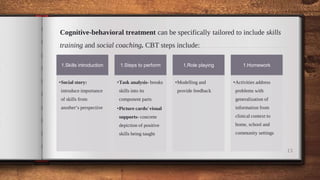
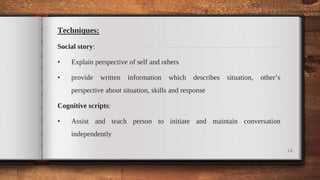
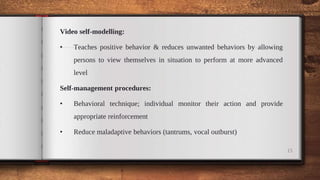
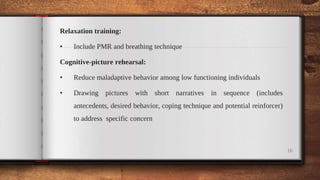
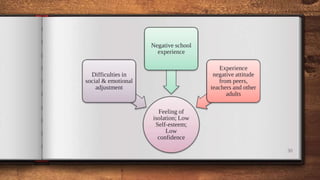
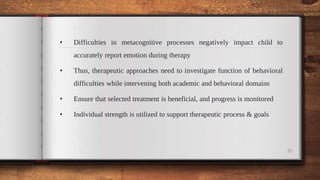
The document provides comprehensive guidelines for clinicians working with children and adolescents with disabilities, focusing on tailored psychotherapeutic services that consider individual needs and comorbid issues. It emphasizes various therapeutic approaches, including cognitive-behavioral treatment, parent training, and social skills training, while also addressing special considerations for autism spectrum disorder, intellectual disabilities, learning disabilities, and traumatic brain injury. The importance of a multifaceted assessment and the role of family involvement in therapy are also highlighted as crucial for effective treatment outcomes.