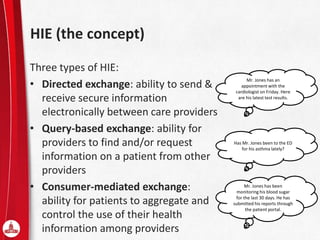
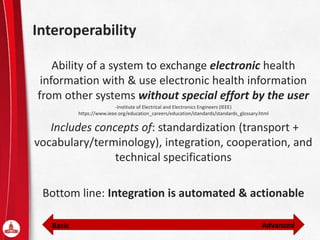
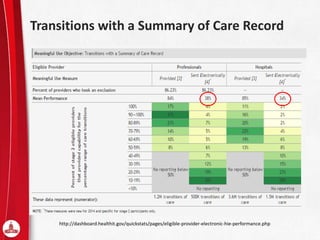
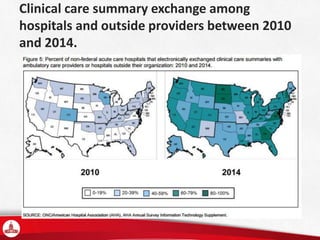
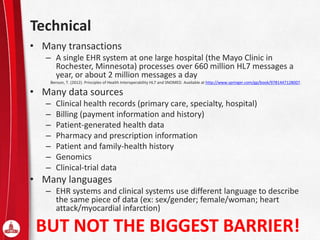
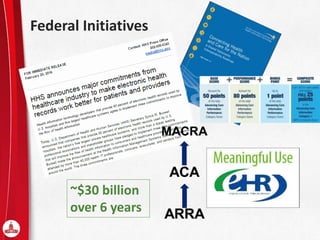
The document discusses the challenges and current status of interoperability in healthcare, distinguishing it from health information exchange (HIE) and highlighting barriers like technical, business, and moral factors. Key concepts include various forms of HIE, the importance of electronic health records (EHR), and state and federal initiatives to improve health information exchange across systems. It emphasizes that while many organizations discuss interoperability, achieving it remains complex and underutilized across the healthcare landscape.