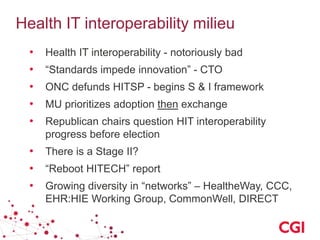
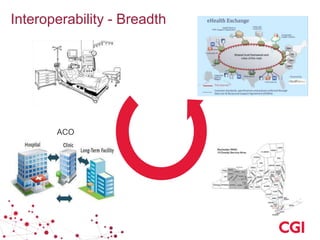
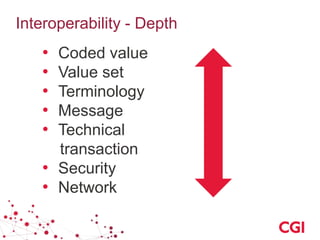
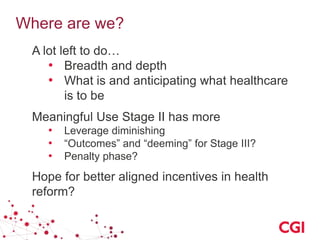
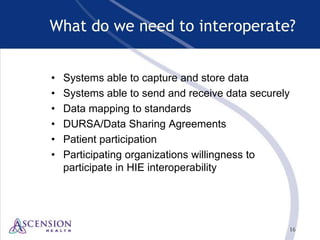
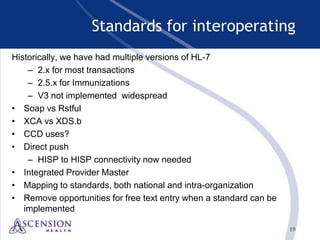
The document discusses achieving interoperability in health IT systems. It describes the current state of interoperability as poor. It outlines key aspects of interoperability including data exchange, system portability, supporting infrastructure, shared functions, and coordinated care information. The document also discusses the process for inducing interoperability, including using incentives, documenting requirements, identifying standards, implementation guidance, and testing. It notes there is still significant work remaining to expand interoperability in terms of breadth across organizations and depth of clinical data elements.