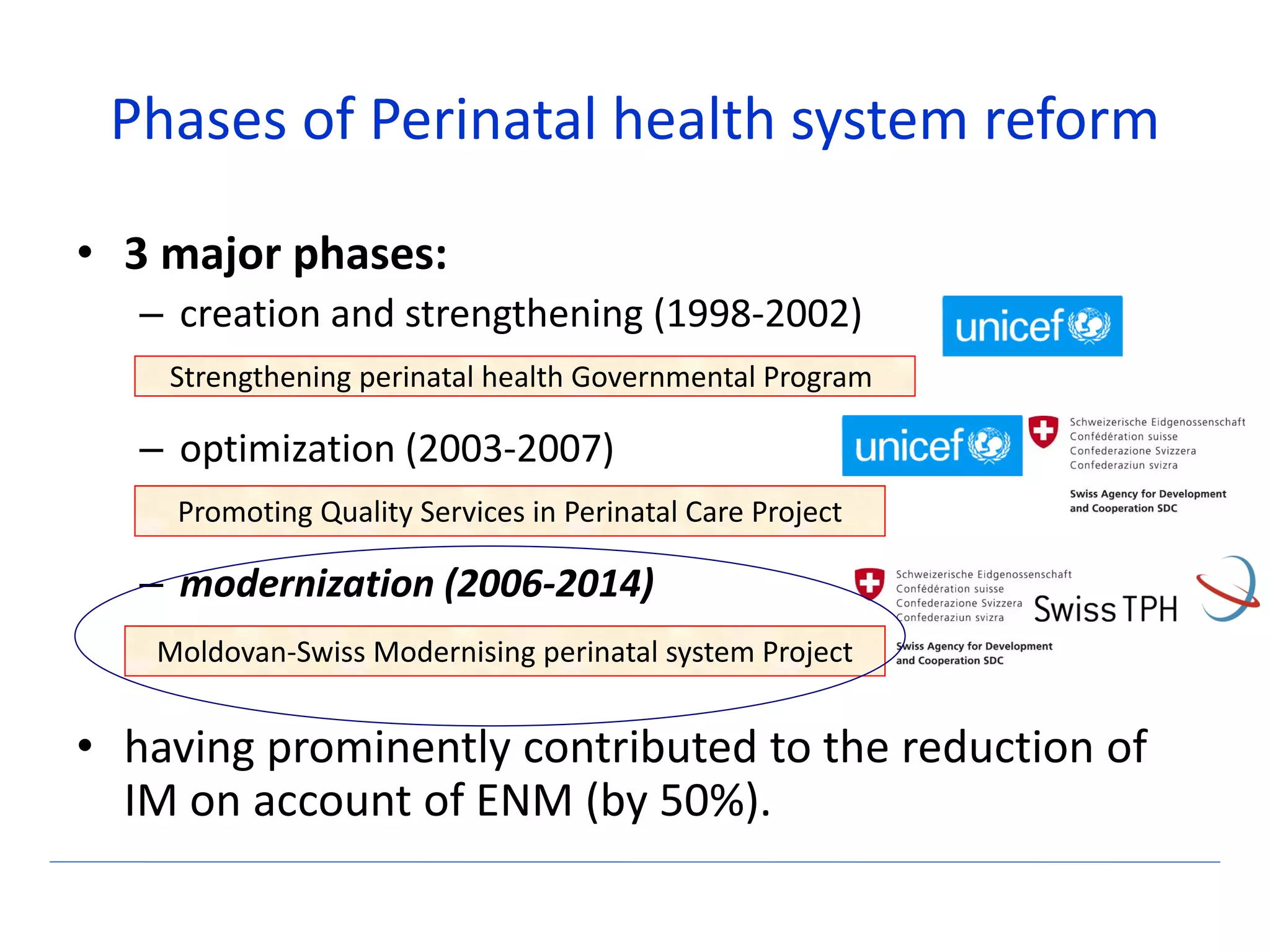
The document discusses the implementation of interdisciplinary simulation training for obstetric and neonatal emergencies in Moldova, highlighting key phases of perinatal health system reform. It outlines the planning, preparation, training stages, and the outcomes of simulation courses conducted for medical professionals, focusing on improving skills and reducing infant mortality. The training has engaged a significant number of specialists and emphasizes ongoing improvements and future training initiatives in the field.