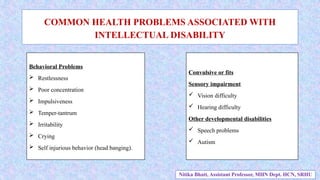
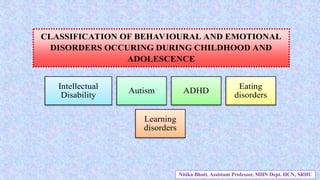
The document discusses behavioral and emotional disorders in children and adolescents, highlighting the importance of early identification and intervention by healthcare workers, particularly nurses. It provides an overview of the ICD-11 classification of disorders such as intellectual disability, autism, and ADHD, and outlines their developmental characteristics, causes, and associated health problems. Additionally, it emphasizes the need for comprehensive assessments and individualized nursing care strategies to support affected individuals and their families.


![DEFINITION
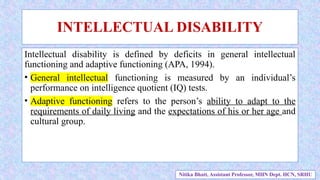
Intellectual disability is defined as a “disorder with onset during the developmental
period that includes both intellectual and adaptive functioning deficits in
conceptual, social and practical domains.
1. Conceptual – language, reading, writing, math, reasoning, knowledge, memory.
2. Social – empathy, social judgment, communication skills, the ability to follow
rules and the ability to make and keep friendships.
3. Practical – independence in areas such as personal care, job responsibilities,
managing money, recreation and organizing school and work tasks.
American Psychiatric Association [APA], 2013
Nitika Bhatt, Assistant Professor, MHN Dept. HCN, SRHU](https://image.slidesharecdn.com/1-240815114703-d639acab/85/Intellectual-disability-Childhood-disorder-8-320.jpg)