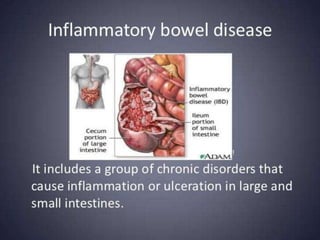
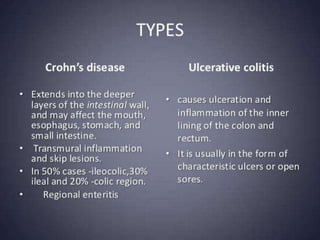
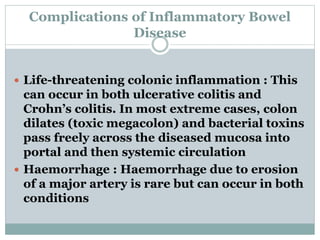
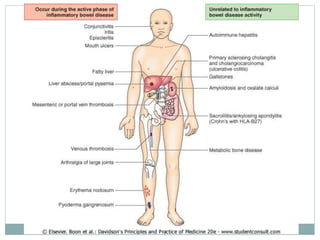
This document discusses inflammatory bowel disease and its complications. Some key complications discussed include life-threatening colon inflammation known as toxic megacolon, hemorrhaging from eroded arteries, and fistulae which are specific to Crohn's disease. Patients with longstanding colitis are also at higher risk for colon cancer. Investigations into IBD include bacteriology tests of stool samples, endoscopy of the bowel, and radiological exams like MRI enterography or CT scans to evaluate disease activity and complications.