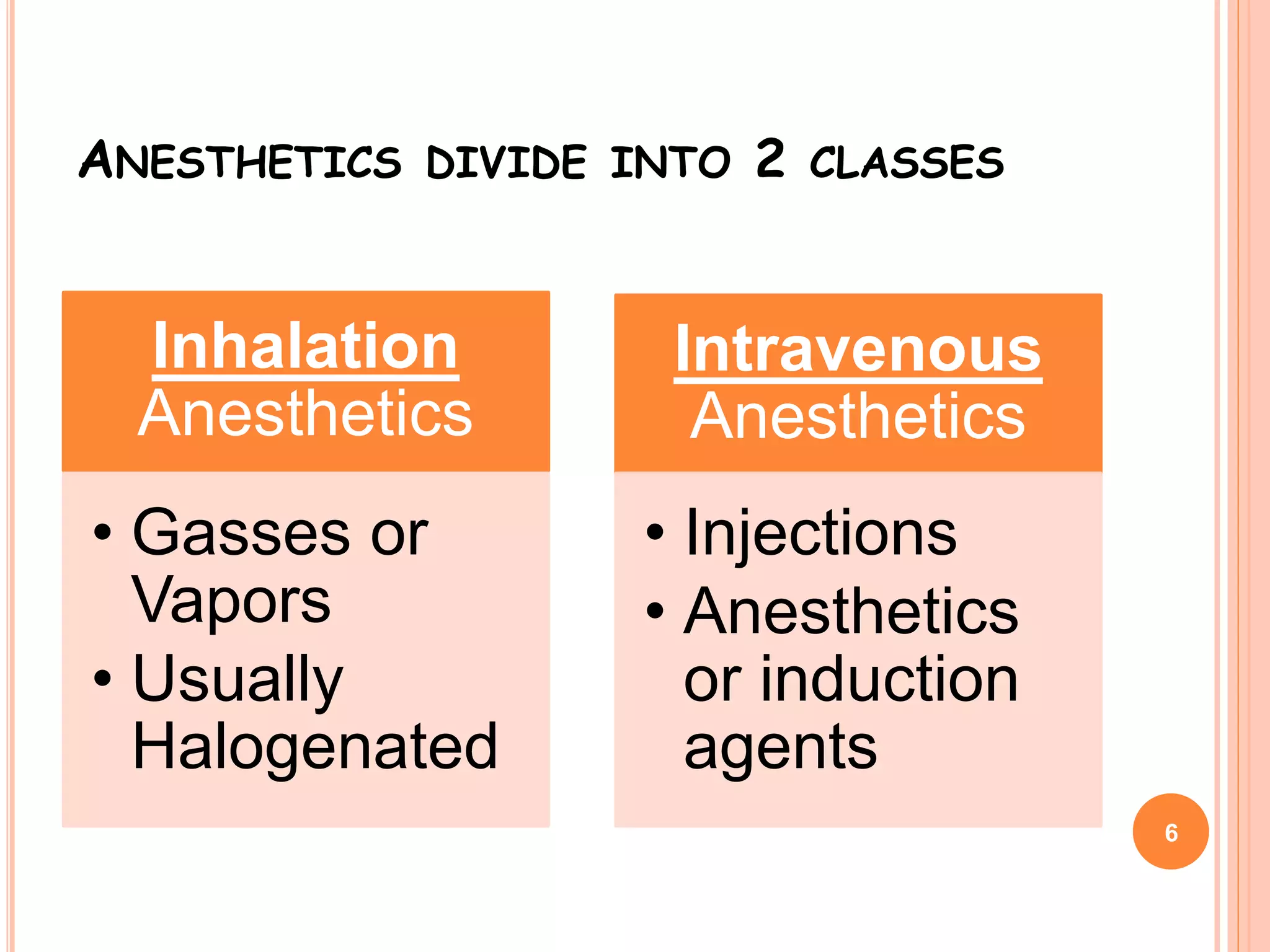
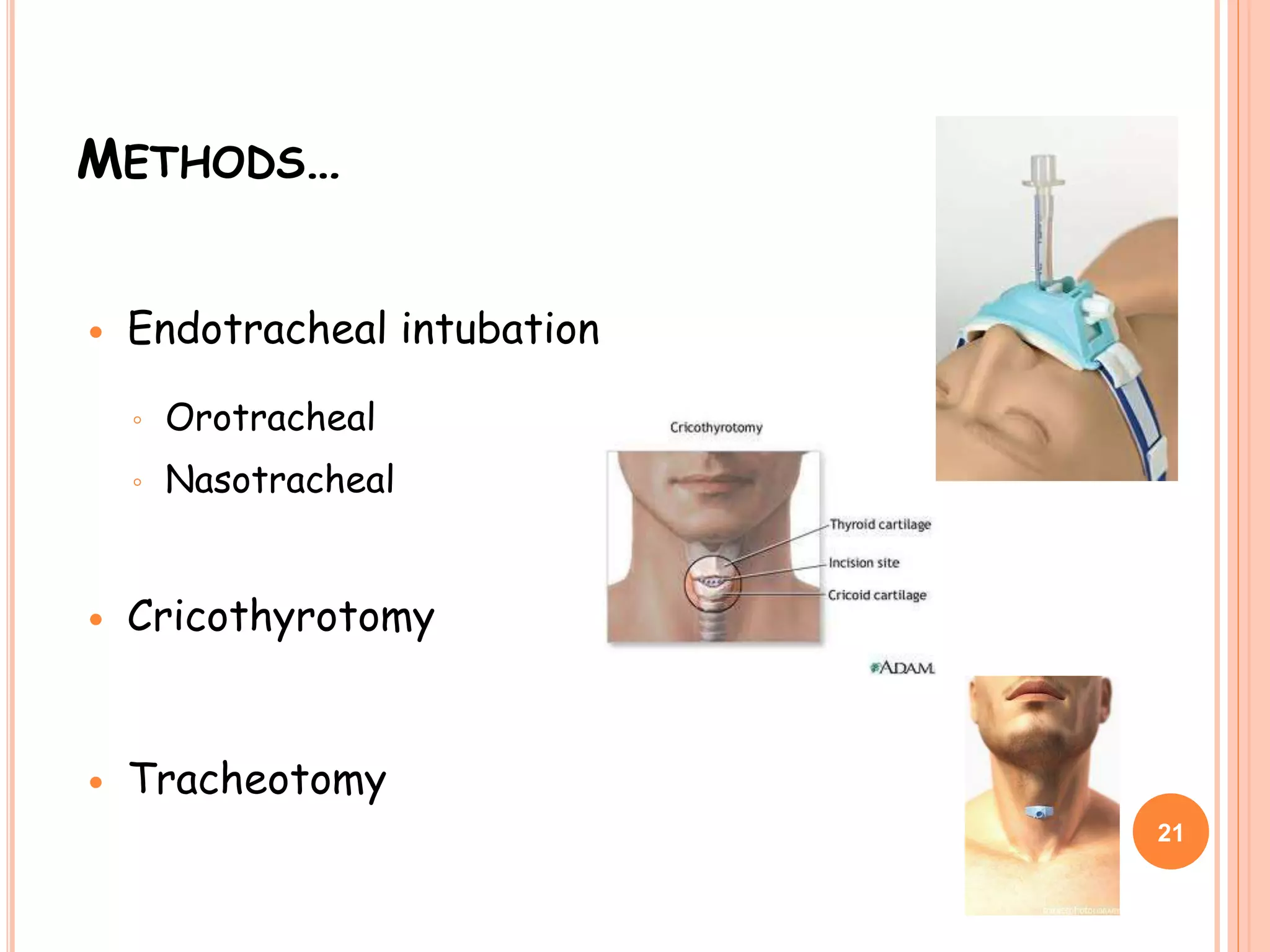
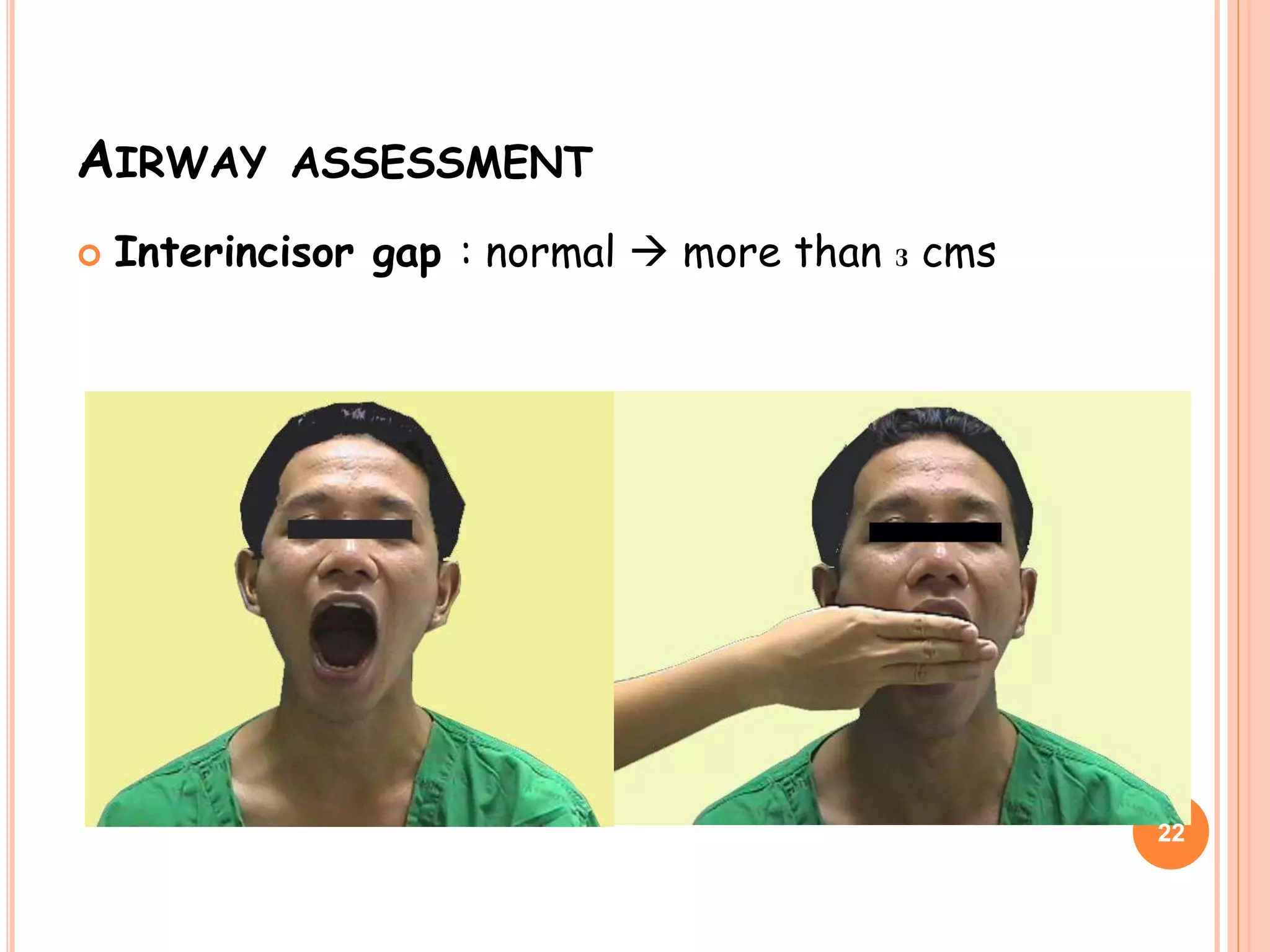
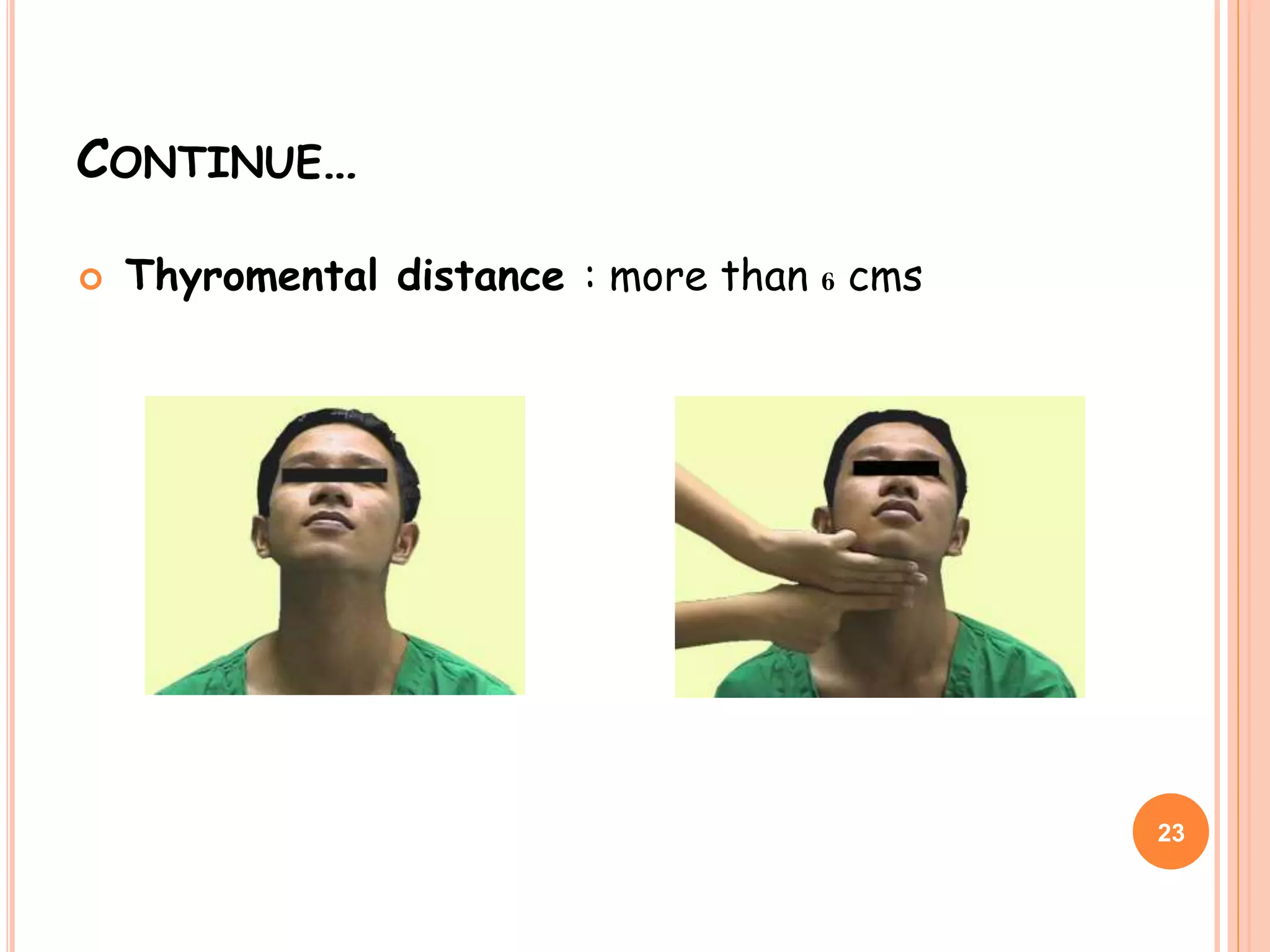
This document provides an overview of induction of anesthesia. It defines inhalation and intravenous induction, describes how anesthesia is maintained, and covers topics like tracheal intubation, neuromuscular agents, emergence and recovery from anesthesia. Anesthetics are divided into inhalation agents administered via gas and intravenous induction agents. Total intravenous anesthesia administered solely by IV is also discussed. Careful patient assessment and monitoring is important for safe induction, maintenance and emergence from anesthesia.