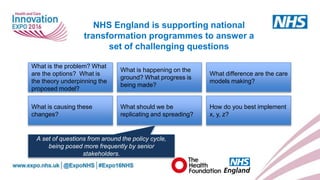
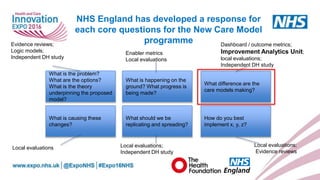
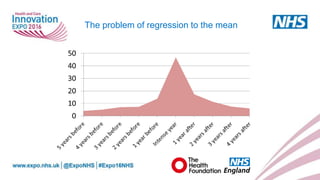
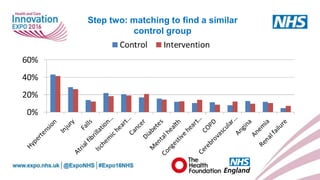
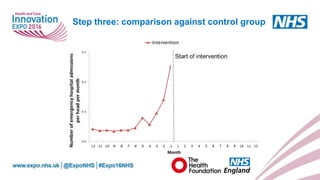
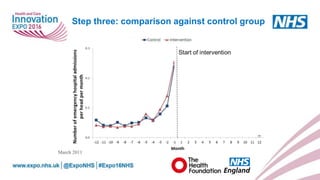
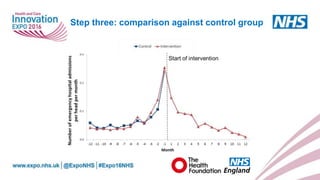
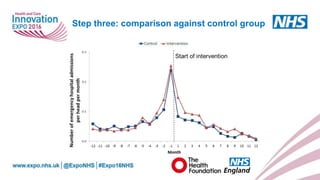
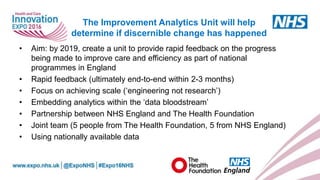
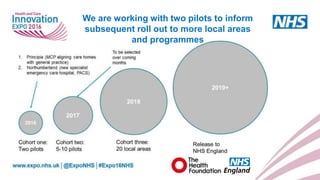
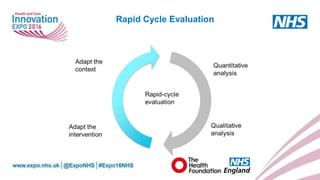
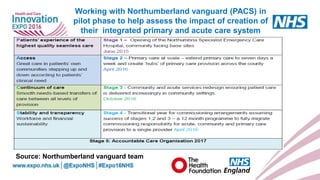
The document describes a workshop on using data analytics to improve healthcare delivery and efficiency. It discusses the challenges of assessing innovations, and introduces the Improvement Analytics Unit, a partnership between NHS England and The Health Foundation to provide rapid feedback on national healthcare programs. The unit will use nationally available data and work with local areas on evaluations to help determine if changes have occurred as a result of various interventions.