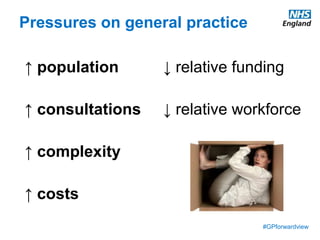
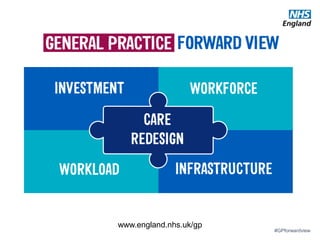
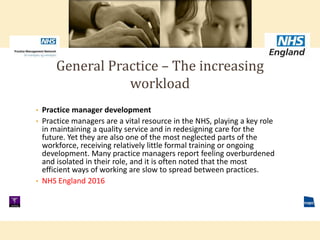
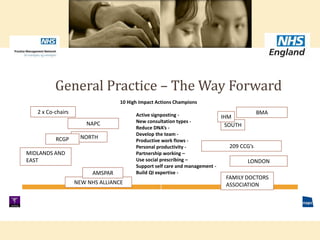
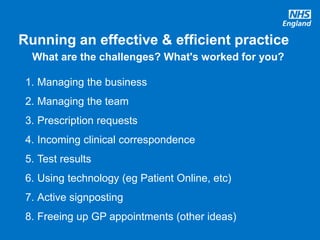
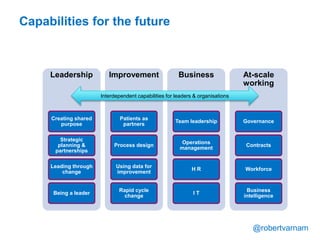
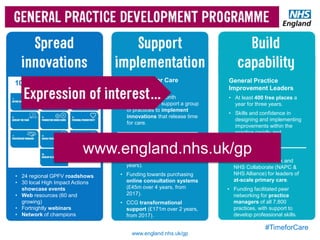
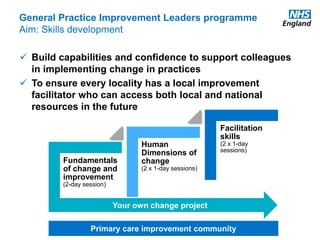
The document discusses a meeting to provide development and support for general practice managers, covering topics such as managing workload in general practices, sharing challenges and solutions, professional development opportunities, and leading primary care into the future. Attendees include representatives from various NHS organizations focused on supporting general practice. The document emphasizes the importance of practice managers sharing their knowledge and experiences to help their colleagues and promote excellence in primary care.