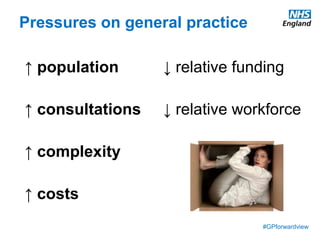
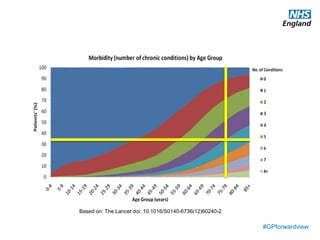
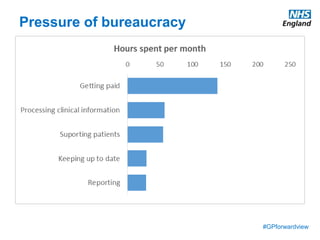
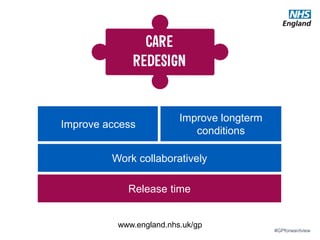
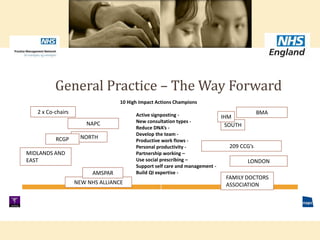
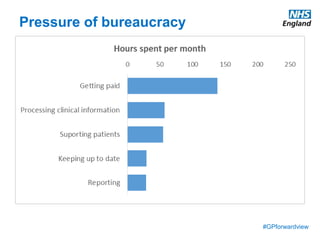
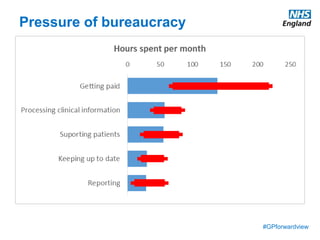
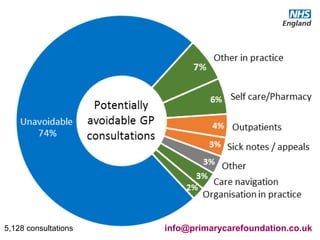
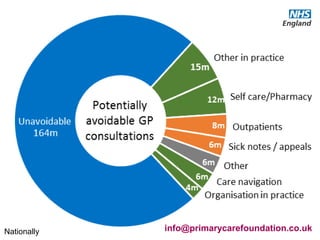
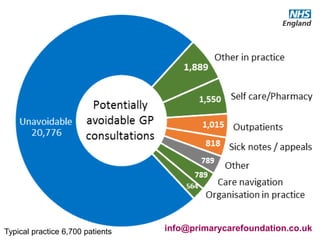
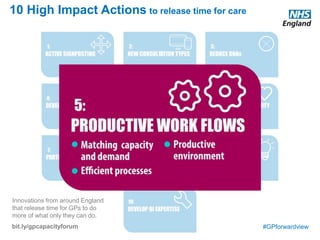
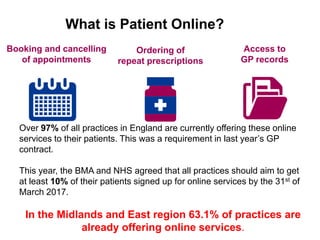
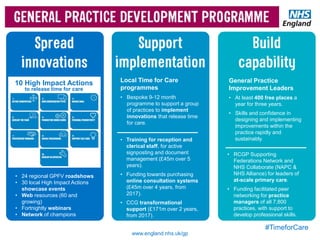
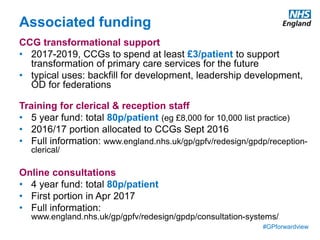
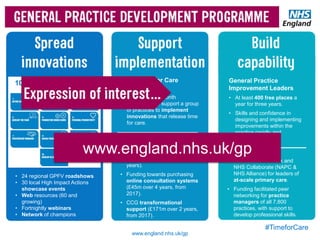
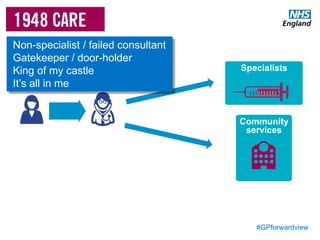
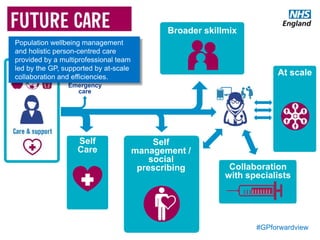
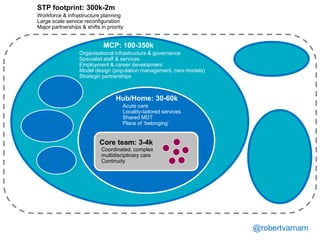
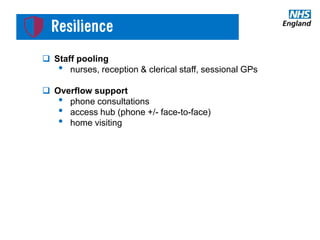
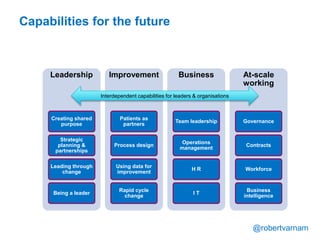
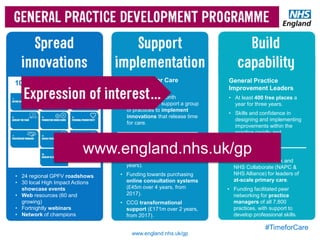
The document discusses managing workload in general practice. It identifies some of the biggest challenges as the increasing pressure on practices from a growing and aging population, rising costs, and increasing bureaucracy. It discusses the GP Forward View's focus on improving access to care, long-term conditions management, and collaborative working. The document then summarizes some approaches practices are taking to better manage workload, such as introducing new ways of working to reduce wasted time, matching capacity to demand, improving processes, creating a more productive environment, supporting self-care, prevention initiatives, online services to streamline tasks, and more proactive long-term condition management.