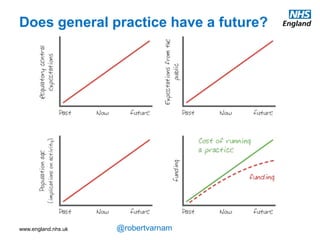
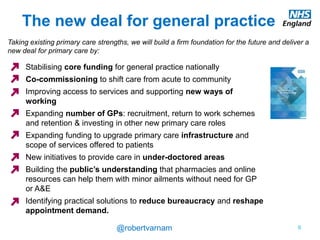
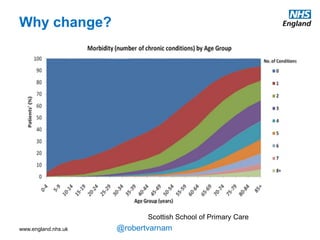
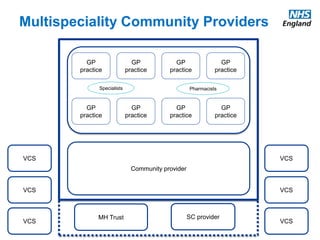
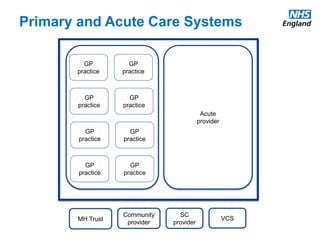
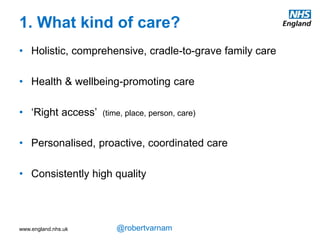
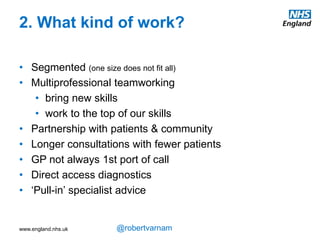
The document discusses the future of general practice in the UK. It notes that while general practice is currently constrained and facing challenges, there are reasons for optimism going forward. New funding, workforce growth, and infrastructure improvements are helping to deliver a new deal for general practice. However, simply doing more of the same is not enough - qualitative changes are needed to better serve patients with long-term conditions. New organizational forms and care models are being implemented to help general practice realize its full potential and meet future needs.