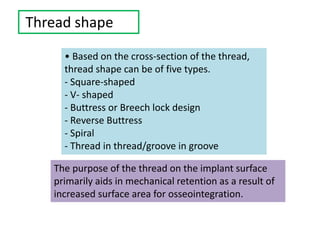
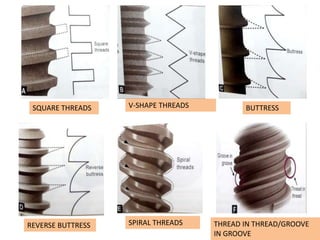
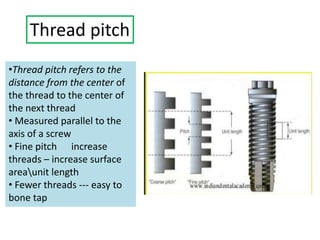
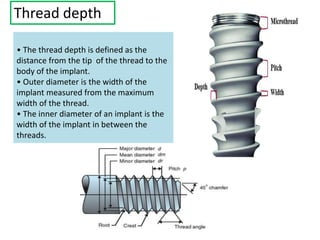
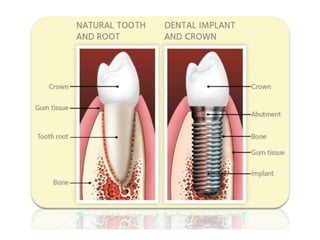
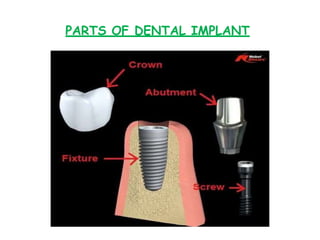
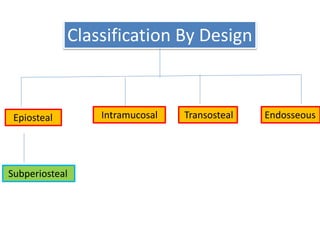
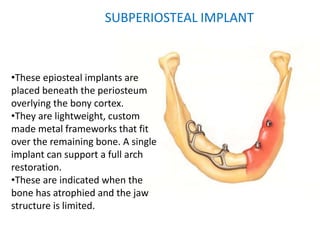
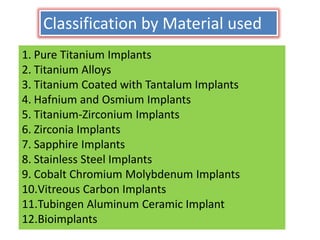
This document outlines the history, design, classification, advantages, and disadvantages of dental implants, emphasizing their role in restoring missing teeth and improving dental function. Key topics include implant types such as endosseous and subperiosteal implants, materials used (like titanium and zirconia), and the advancements made in implant technology over the centuries. Additionally, it discusses the rationale for using implants over traditional dental prosthesis, highlighting their stability, comfort, and aesthetic benefits.






![Tapered hexagon
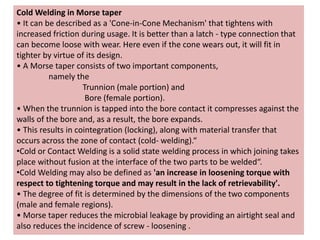
• The tapered hexagon connection has six
sides with 1.5-degree taper.
• It also has a corresponding close
tolerance hexagonal abutment recess that
can be friction-fit onto the hex.
• This system is also known as the Hex
Lock Innovation.
• Features:
Increased abutment stability and
accurate transfer procedure.
Claims to have zero micromotion at the
implant abutment junction.
[Examples, Spectra implant systems,
Swede-Vent TL (Paragon Implant Co.,
Encino,CA)].](https://image.slidesharecdn.com/basicaspectsofdentalimplants-200704035448/85/Basic-aspects-of-dental-implants-71-320.jpg)