This document discusses different types of hypersensitivity and immune responses. It covers:
1. The four main types of hypersensitivity reactions (Type I-IV) based on their immune mechanisms, examples of each type, and their characteristic features.
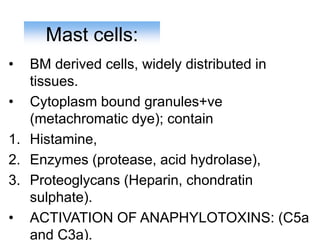
2. Details on Type I immediate hypersensitivity and anaphylaxis, including primary and secondary mediators, mast cell activation, and atopic susceptibility.
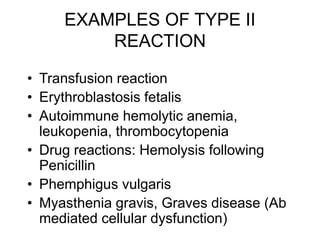
3. Type II antibody-mediated hypersensitivity, examples like hemolytic anemia, and mechanisms of tissue damage.
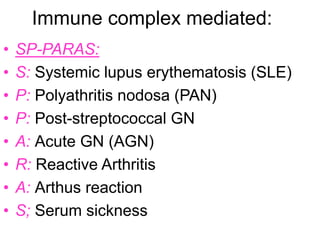
4. Type III immune complex-mediated hypersensitivity, examples like SLE, and mechanisms of inflammation and tissue damage.
5. Type IV delayed hypersensitivity, using tuberculosis as an