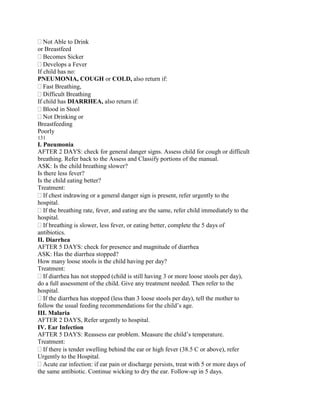
This document provides a summary of a facilitator's guide for a Community-Integrated Management of Childhood Illness (C-IMCI) manual. The manual is divided into two sections: the first covers assessing, classifying, and determining appropriate actions for various diseases and prevention activities; the second provides home care treatment and follow-up guidelines. Each chapter in the first section follows a 7-step process including reflection, definition, recognition of signs, skill development, evaluation and management of cases using a recording form, determining appropriate action, and referral procedures. The guide is intended to train community health workers to identify and manage common childhood illnesses in an integrated manner.