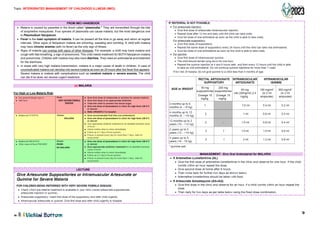
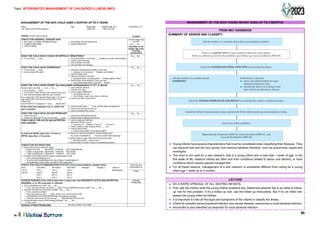
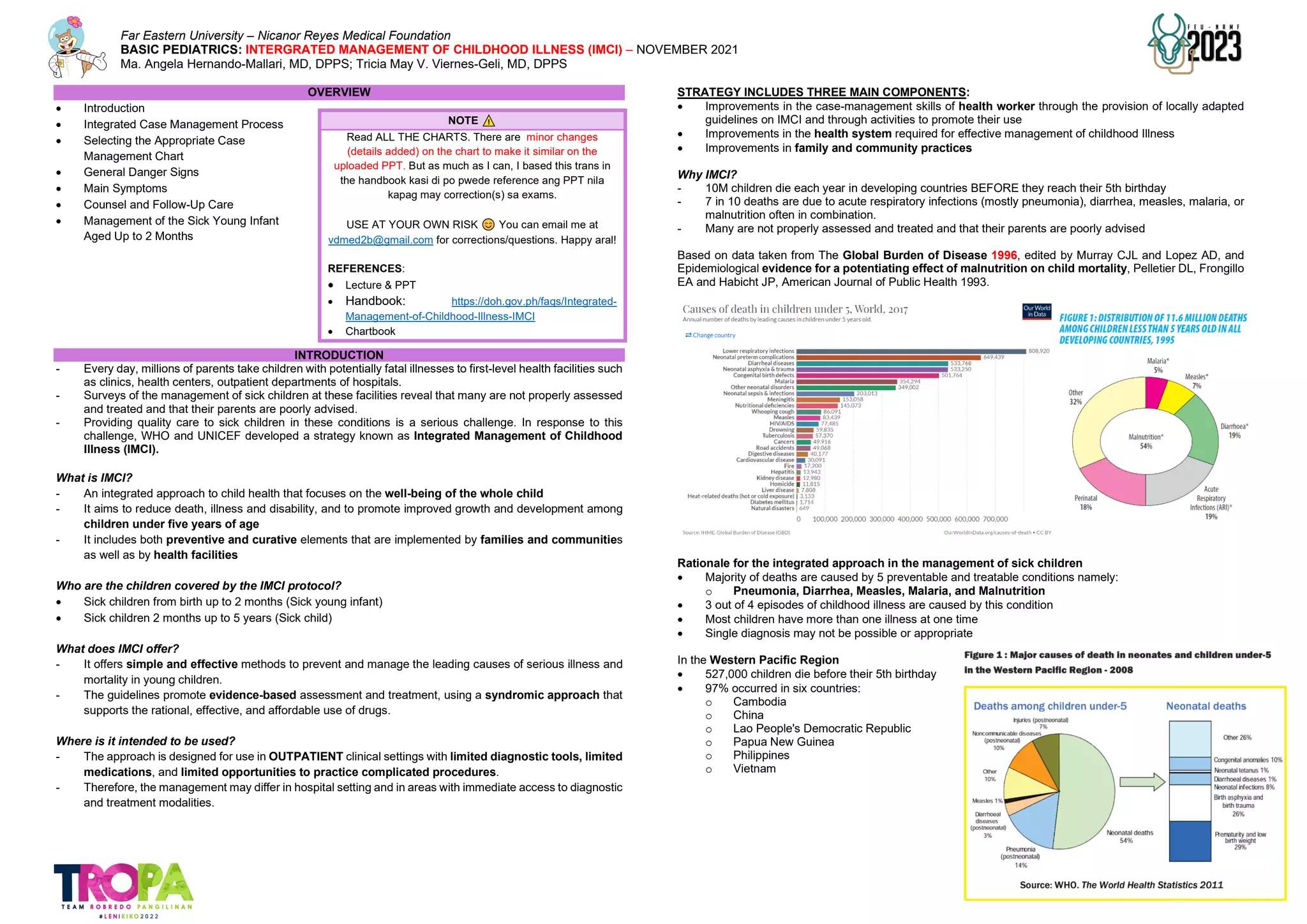
The document provides an overview of Integrated Management of Childhood Illness (IMCI), which is an integrated approach to child health developed by WHO and UNICEF. IMCI focuses on well-being of children under five years old and includes preventive and curative elements implemented by families, communities, and health facilities. The integrated case management process for sick children ages 1 week to 5 years involves assessing and classifying the child's illnesses, identifying specific treatments, providing treatment instructions, counseling the mother, and follow-up care. The goal is to reduce mortality from major childhood illnesses like pneumonia, diarrhea, and malnutrition through improved skills and systems for managing sick children at primary health facilities.




![Topic: INTERGRATED MANAGEMENT OF CHILDHOOD ILLNESS (IMCI)
8
FROM IMCI HANDBOOK + LECTURE
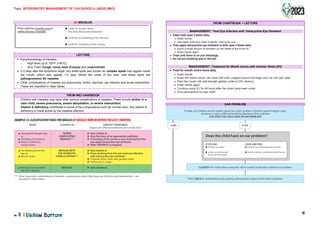
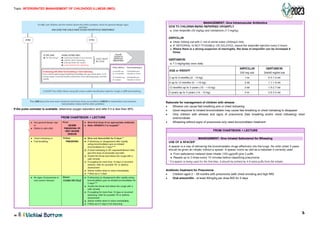
TYPES OF DIARRHEA [REFER TO TABLE BELOW]
• If an episode of diarrhea lasts <14 days, it is acute diarrhea. Acute watery diarrhoea causes
dehydration and contributes to malnutrition. The death of a child with acute diarrhoea is usually due to
dehydration.
• If the diarrhea lasts ≥14 days, it is persistent diarrhea (without dehydration). Up to 20% of episodes of
diarrhea become persistent. Persistent diarrhoea often causes nutritional problems that contribute to
deaths in children who have diarrhea. If there is dehydration, classify it as severe persistent diarrhea.
o Advise the mother on feeding give multivitamins and minerals including ZINC for 14 days and follow
up in five days.
• Diarrhea with blood in the stool, with or without mucus, is called dysentery. The most common
cause of dysentery is Shigella bacteria. Amoebic dysentery is not common in young children. A child
may have both watery diarrhoea and dysentery.
o Management: Ciprofloxacin for three days and advice to follow up in three days.
Treatment for Diarrhea
• Use of low/reduced osmolarity Oral Rehydration
Salts (ORS)
• Providing children with zinc for 14 days
− Children > 6 months 20 mg zinc
− Children < 6 months 10 mg of zinc
• Ciprofloxacin as first line drug for bloody diarrhea
Composition of the old and reformulated ORS
- New/reformulated has low or reduced osmolarity.
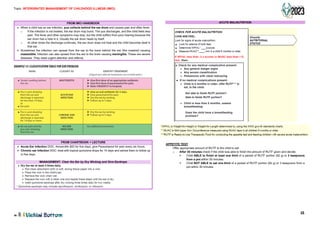
FEVER
LECTURE
• Fever is defined by history of ‘feels hot’ or a temperature of ≥37.5° C based on axillary temperature.
• Rectal temperature is approximately 0.5° C higher
• Decide if the child is high risk or low risk for malaria. There’s separate table for HIGH malaria risk.
• Also, look for bacterial cause of fever (e.g., local tenderness, oral sores, refusal to use a limb, hot tender
swelling, red tender skin or boils, lower abdominal pain or pain in passing urine in older children.
• If no malaria test is available in a HIGH risk area, classify it as malaria. In low malaria risk and no obvious
cause of fever classify as malaria.
MALARIA RISK AREA: Palawan, Davao Del Sur, Davao Del Norte, Sultan Kudarat, Sulu archipelago
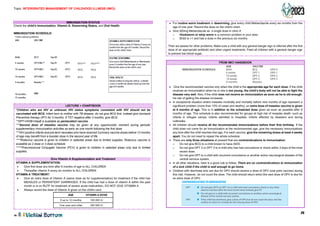
NOTE
In Vitamins and Minerals lecture:
• WHO recommends zinc supplementation to
all cases of diarrhea and dysentery
• Given for 10-14 days
I I
.FOR DYSENTERY give Ciprofloxacine
FIRST-LINE ANTIBIOTIC: Oral Ciprofloxacine
CIPROFLOXACINE
AGE Give 15mg/kg two times daily for 3 days
250 mg tablet I 500 mg tablet
Less than 6 months 1/2 I 1/4
6 months uo to 5 vears 1 I 1/2
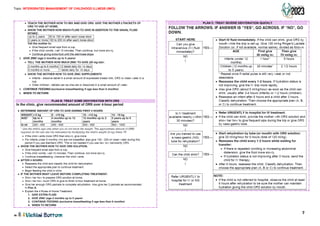
SIGNS CLASSIFY AS IDENTIFYTREATMENT
(Urgent pre-referral treatments are in bold print.)
• Dehydration present SEVERE ► Treat dehydration before referral unless the child has
PERSISTENT another severe classification.
DIARRHOEA ► Refer to hospital.
• No dehydration PERSISTENT ► Advise the mother on feeding a ch ild who has
DIARRHOEA PERSISTENT DIARRHOEA.
► Follow-up in 5 days.
• Blood in the stool DYSENTERY ► Treat for 5 days with an oral antibiotic
recommended for Shigella in your area.
► Follow-up in 2 days.
r·-----------------------1
I
I
I
I
I I
'-------------------------~
OLD WHO- Rebnnulated
ORS (meq ORS (meqor
ormmol/I) mmol/I)
Glucose 111 75
Sodium 90 75
Chloride 80 65
Potassium 20 20
Citrate 10 10
Osmolarity 311 245
••/ickil,i Bottom
For ALL sick children ask the mother about the child's problem, check for general danger signs, ask
about cough or difficult breathing, diarrhoea and then
ASK: DOES THE CHILD HAVE FEVER?
Does the child have fever?
(by history or feels hot or temperature 37.5 °C** or above)
IF YES:
Decide the Malaria Risk: high or low
THEN ASK:
• For how long?
• If more than 7 days, has
fever been present every day?
• Has the ch ild had measles within
the last 3 months?
If the child has measles now or
within the last 3 months:
LOOKAND FEEL:
• Look or feel for stiff neck.
• Look for runny nose.
Look for signs of MEASLES
• Generalized rash and
• One of these: cough, runny nose,
or red eyes.
• Look for mouth ulcers.
Are they deep and extensive?
• Look for pus draining from the eye.
• Look for clouding of the cornea.
Do malaria test: If no severe
classification
• In all fever cases with
HIGH MALARIA RISK
• In LOW malaria risk if no
obvious cause of fever
present.
CLASSIFY the child's illness using the colour-coded classification tables for fever.
Then ASKabout the next main symptom: ear problem, and CHECK for malnutrition and anaemia,
immunization status and for other problems.
r-------------------------------------------------------1
--------------------------------------------------------](https://image.slidesharecdn.com/basic-pedia-lec-imci-version-4-230208045628-b25e8f71/85/BASIC-PEDIA-Lec-IMCI-Version-4-pdf-8-320.jpg)