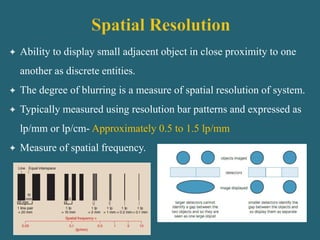
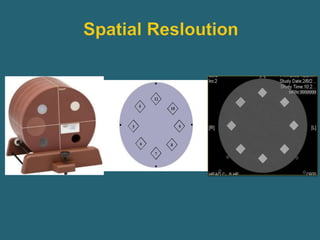
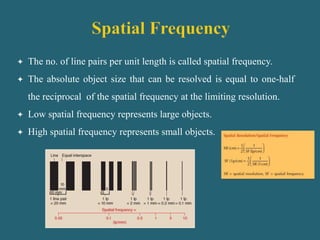
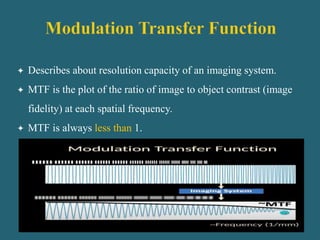
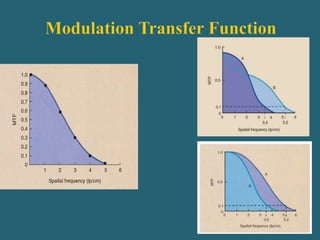
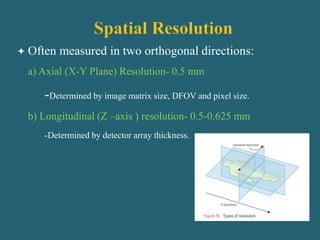
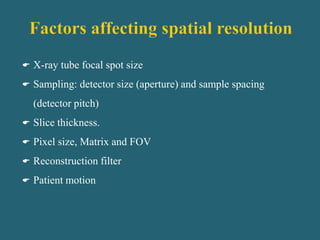
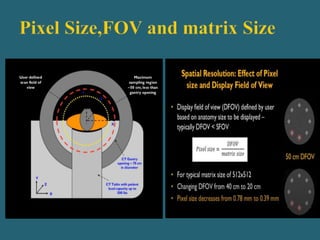
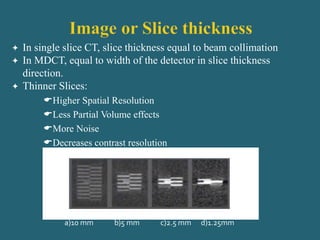
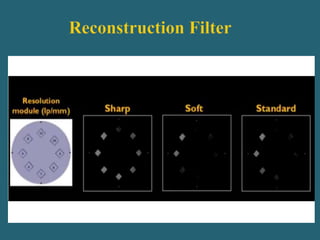
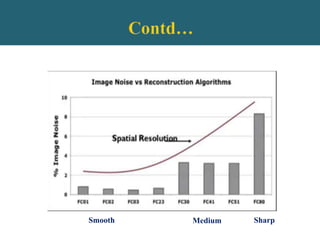
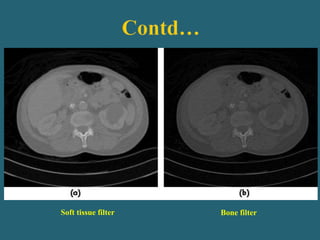
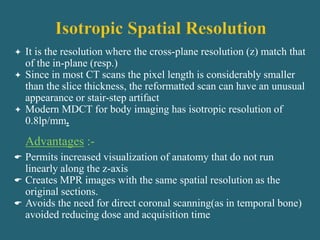
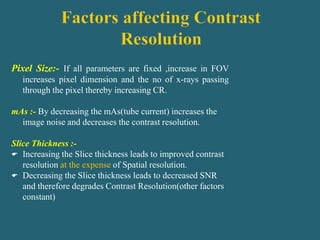
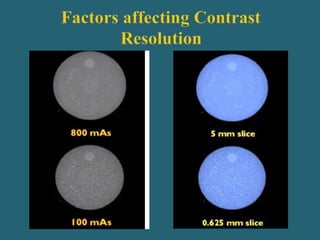
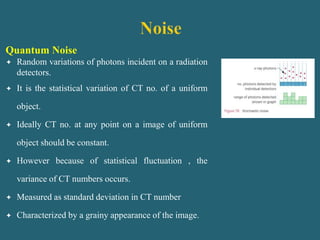
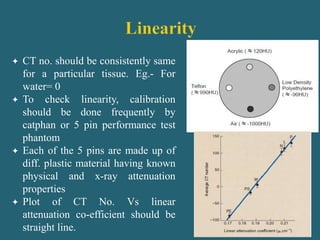
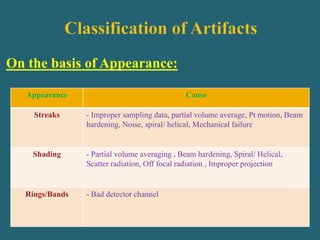
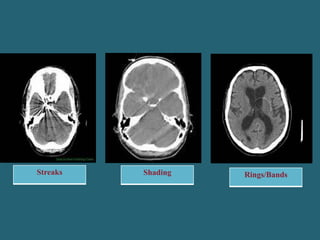
This document discusses factors that influence image quality in CT imaging. It describes several key factors that determine spatial resolution, contrast resolution, and other quality metrics. Spatial resolution is influenced by pixel size, slice thickness, reconstruction filter, and other technical parameters. Contrast resolution depends on factors like mAs, slice thickness, and patient size. Image noise arises from quantum and electronic effects and is reduced by increasing mAs and slice thickness. Artifacts can also degrade image quality. Overall, the document provides an overview of technical imaging factors and how they impact different elements of image quality in CT.