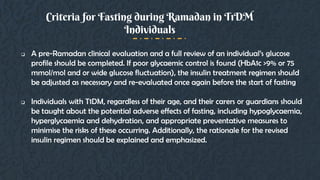
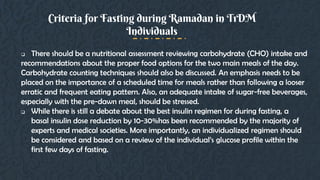
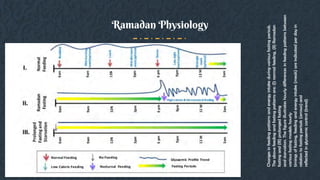
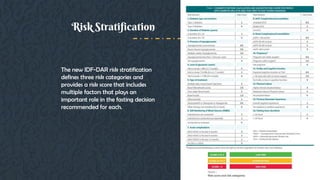
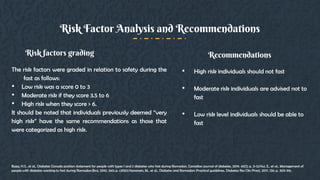
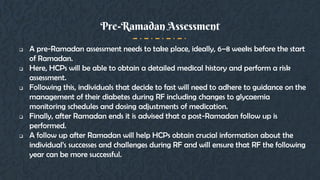
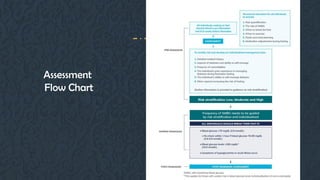
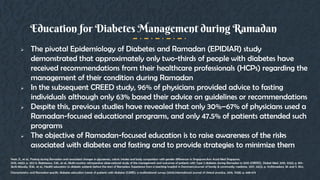
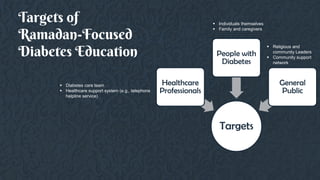
This document provides guidelines for managing diabetes during Ramadan. It discusses the growing prevalence of diabetes in Muslim-majority countries and regions. Fasting during Ramadan can impact blood sugar levels and increase risks for diabetics like hypoglycemia and hyperglycemia. The document outlines the physiological changes that occur during the Ramadan fast and lifestyle adjustments. It also provides a risk stratification system for diabetics fasting based on risk factors. The guidelines recommend a pre-Ramadan assessment, education on diabetes management during fasting, and post-Ramadan follow-up. Both medical and religious perspectives on fasting for diabetics are considered to develop balanced recommendations.



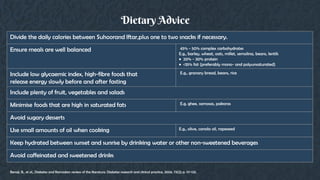
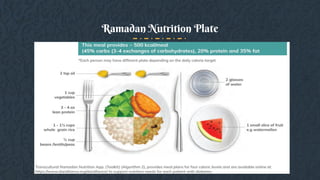
![The main aims of MNT during Ramadan fasting are to ensure that:
Individuals with diabetes consume an adequate amount of calories, with
balanced proportions of macronutrients, during the non-fasting period
(i.e., sunset to dawn) to prevent hypoglycaemia during the fasting period.
Individuals with diabetes equally distribute their carbohydrate intake
among meals to minimize postprandial hyperglycaemia.
Individuals with diabetes and HCPs give consideration to comorbidities
such as hypertension and dyslipidaemia when formulating MNT plans.
Aims
DAR Alliance,; Available from:www.daralliance.org/daralliance.Hamdy, O., et al., The Ramadan Nutrition Plan (RNP) for Patients with Diabetes. Diabetes
and Ramadan: practical guidelines [Internet], 2017: p. 73-83.Bravis, V., et al., Ramadan Education and Awareness in Diabetes (READ) programme for Muslims
with Type 2 diabetes who fast during Ramadan.Diabetic Medicine, 2010. 27(3): p. 327-331](https://image.slidesharecdn.com/idfdar2021-ud-210304071454/85/Idf-dar-2021-ud-36-320.jpg)
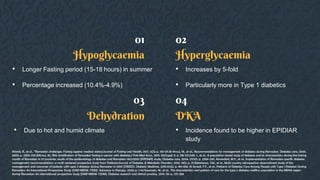
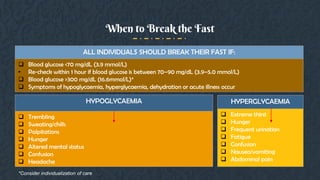
![ Hypoglycaemia, especially during the late period of fasting before Iftar;
Severe hyperglycaemia after each of the main meals;
Dehydration, especially in countries with longer fasting hours and hot
climates;
Significant weight gain due to an increased caloric intake and a reduction in
physical activity;
Electrolyte imbalances;
Acute renal failure in individuals prone to severe dehydration, particularly
the elderly and those with impaired kidney function.
Diabetes-related Risks during Ramadan
DAR Alliance,; Available from:www.daralliance.org/daralliance.Hamdy, O., et al., The Ramadan Nutrition Plan (RNP) for Patients with Diabetes. Diabetes
and Ramadan: practical guidelines [Internet], 2017: p. 73-83.Bravis, V., et al., Ramadan Education and Awareness in Diabetes (READ) programme for Muslims
with Type 2 diabetes who fast during Ramadan.Diabetic Medicine, 2010. 27(3): p. 327-331](https://image.slidesharecdn.com/idfdar2021-ud-210304071454/85/Idf-dar-2021-ud-37-320.jpg)
![Calorie and Carbohydrate Distributions for the Ramadan Nutrition Plan
DAR Alliance,; Available from:www.daralliance.org/daralliance.Hamdy, O., et al., The Ramadan Nutrition Plan (RNP) for Patients with Diabetes. Diabetes
and Ramadan: practical guidelines [Internet], 2017: p. 73-83.Bravis, V., et al., Ramadan Education and Awareness in Diabetes (READ) programme for Muslims
with Type 2 diabetes who fast during Ramadan.Diabetic Medicine, 2010. 27(3): p. 327-331](https://image.slidesharecdn.com/idfdar2021-ud-210304071454/85/Idf-dar-2021-ud-38-320.jpg)