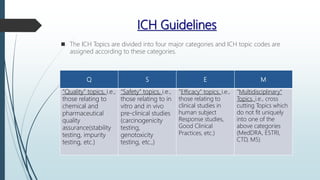
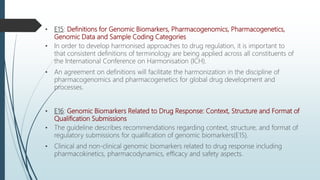
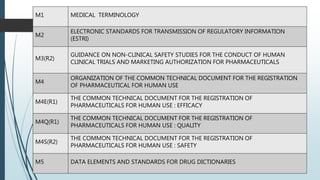
The International Conference on Harmonisation (ICH) brings together regulators and industry representatives from the European Union, Japan, and the United States to discuss scientific and technical aspects of pharmaceutical product registration. The goal of ICH is to promote international harmonization of technical requirements through the development of common guidelines. ICH guidelines cover various topics including quality, safety, efficacy, and multidisciplinary issues. The guidelines provide recommendations on nonclinical studies, clinical trial design and analysis, and the format and content of registration documents to harmonize the technical requirements for pharmaceuticals across ICH regions.