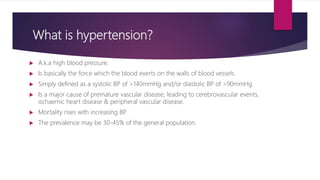
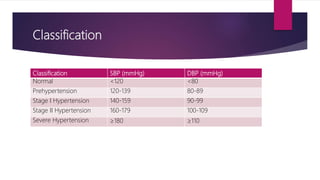
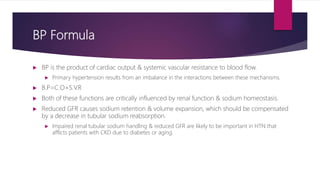
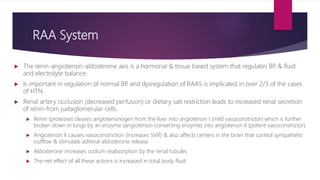
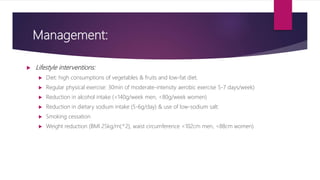
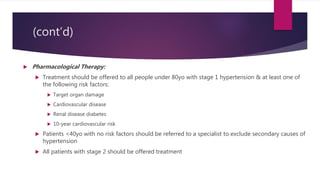
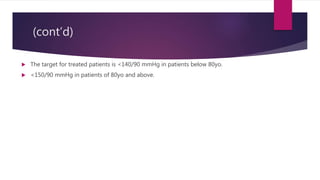
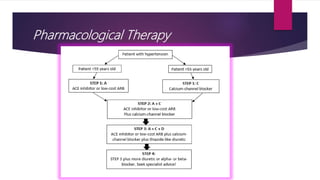
Hypertension (HTN), also known as high blood pressure, is defined as a systolic blood pressure above 140 mmHg or a diastolic blood pressure above 90 mmHg. It is a major cause of heart disease and stroke. The renin-angiotensin-aldosterone system (RAAS) regulates blood pressure and fluid balance and dysregulation of this system is implicated in the majority of hypertension cases. Management involves lifestyle modifications like diet, exercise, weight loss and reducing sodium intake as well as pharmacological therapy with medications that target the RAAS or lower blood pressure directly. The goal of treatment is to lower blood pressure below 140/90 mmHg.