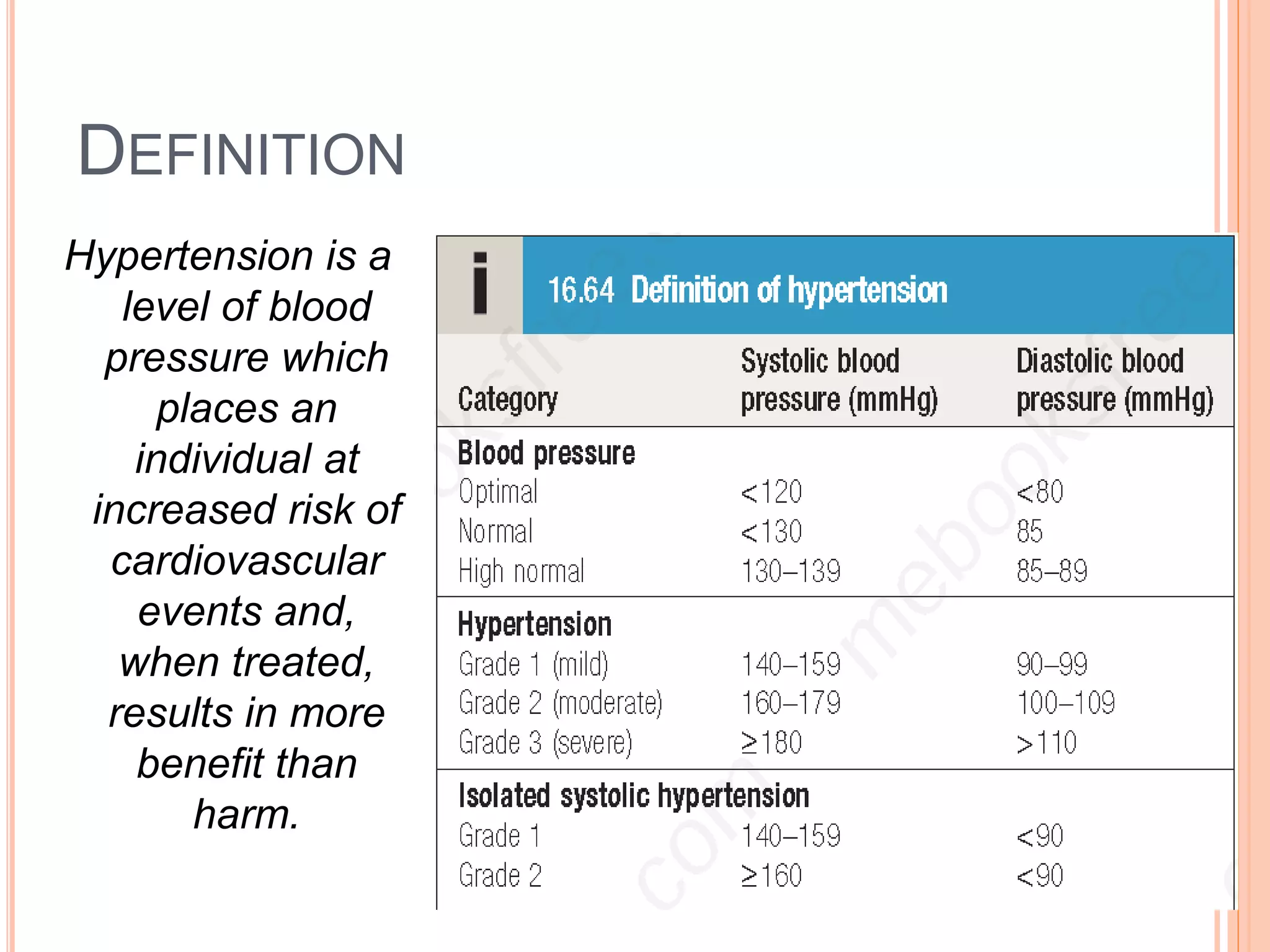
Hypertension is a major global health issue, contributing to millions of deaths and increasing the risk of cardiovascular diseases. The condition can be classified into essential and secondary hypertension, with various genetic, environmental, and lifestyle factors influencing its development. Effective management includes lifestyle changes and pharmacotherapy, while complications may affect multiple organs, necessitating careful monitoring and treatment.