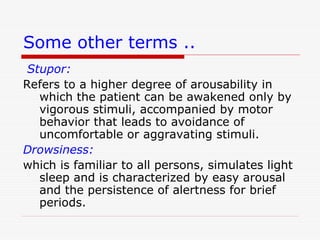
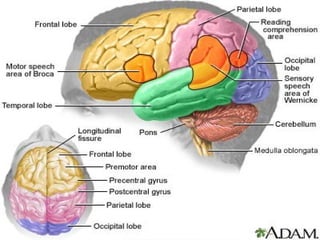
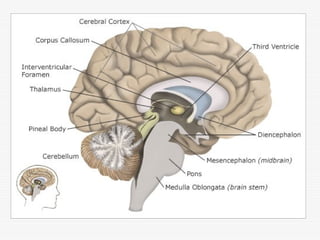
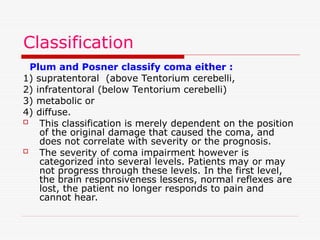
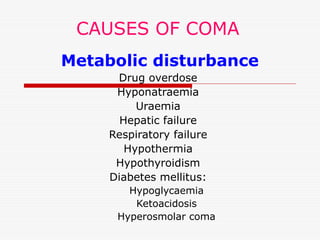
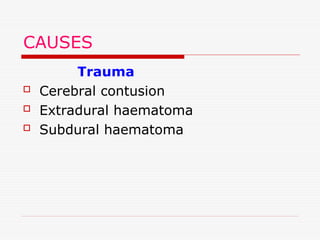
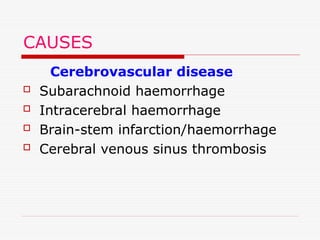
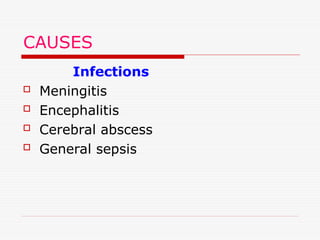
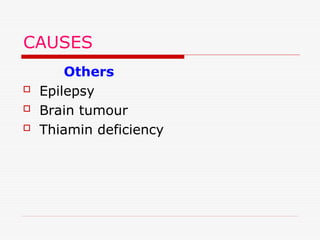
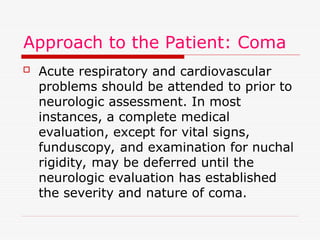
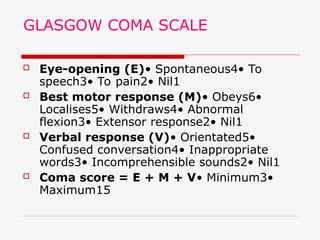
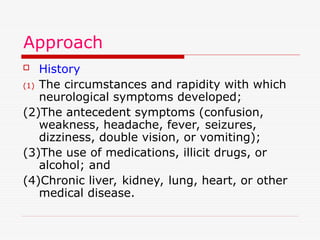
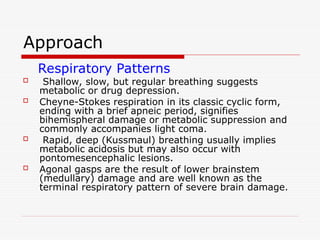
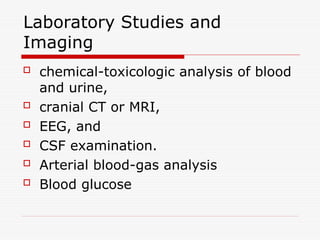
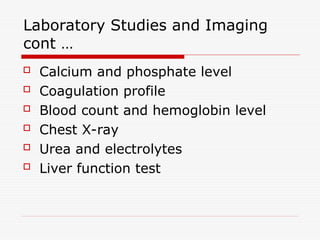
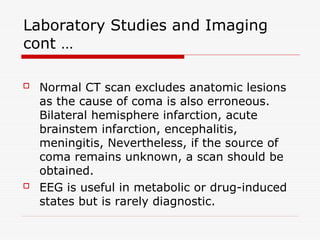
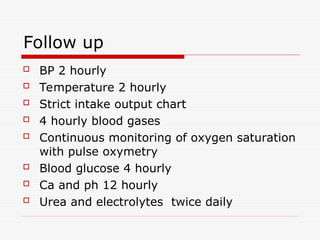
Coma is a state of unconsciousness where a patient cannot respond to their environment, and can be classified into different conditions such as stupor, drowsiness, and vegetative state. It results from damage to the cerebral cortex or the reticular activating system, and may be caused by various factors including metabolic disturbances, trauma, or infections. Treatment involves immediate medical attention to respiratory and circulatory support, prevention of complications, and ongoing monitoring and care.