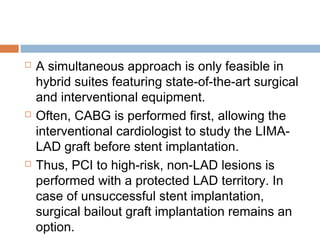
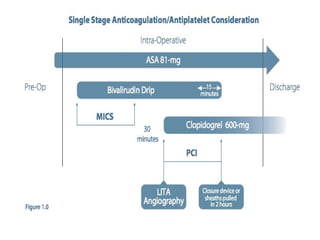
Hybrid coronary revascularization (HCR) combines coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) to treat multivessel coronary artery disease. HCR aims to perform CABG on the left anterior descending artery using a left internal mammary artery graft via minimally invasive surgery while treating other vessels with PCI. This approach seeks to provide the benefits of CABG for the LAD while reducing surgical trauma compared to traditional CABG. The optimal strategy and order of CABG versus PCI, as well as antiplatelet management, are debated due to the lack of large randomized controlled trials on HCR. HCR shows promise for high surgical risk patients but further research is still needed to define appropriate patient selection




















![PATENCY RATES
Fitzgibbon A or B LIMA patency rates (A
[excellent], B [fair], or O [occluded]) have
been reported in a high percentage of
patients: ranging from 93% to 100% of
patients in the perioperative period ,90% and
94% of patients at 6 months and 91% of HCR
patients at 2 years post-grafting.](https://image.slidesharecdn.com/hcr-150311101929-conversion-gate01/85/Hybrid-Coronary-Revascularization-57-320.jpg)