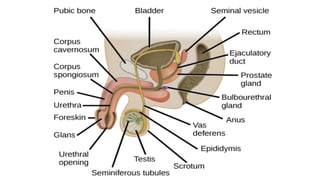
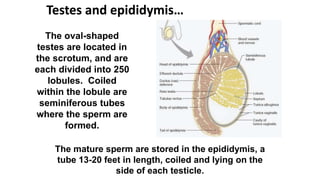
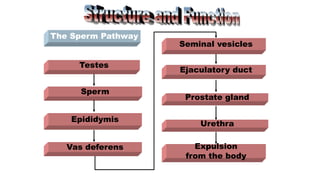
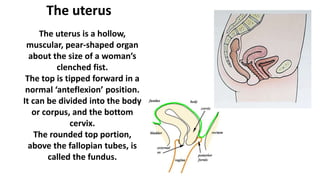
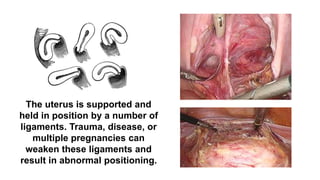
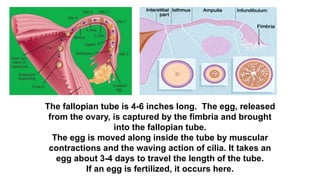
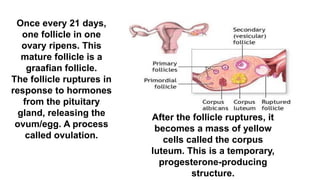
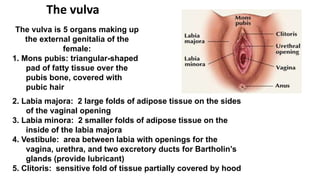
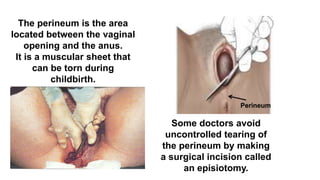
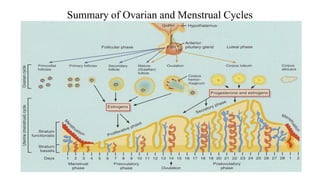
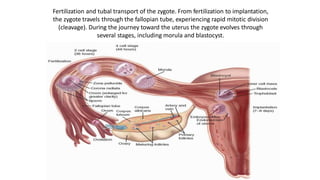
The reproductive systems in males and females consist of both primary and secondary sex organs and glands. The primary function is reproduction through fertilization. The male reproductive system includes external organs like the penis and scrotum, and internal organs like the testes, vas deference, and prostate. Sperm are produced in the testes and travel through the vas deference. The female reproductive system includes external organs like the vulva and internal organs like the ovaries, uterus, cervix, and fallopian tubes. The ovaries produce eggs and the uterus provides nourishment to an embryo during pregnancy. The menstrual cycle regulates female fertility through phases like the follicular, ovulatory, and luteal phases.