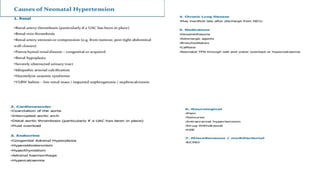
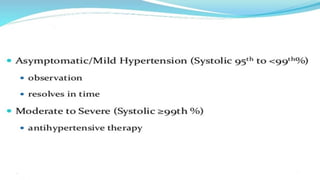
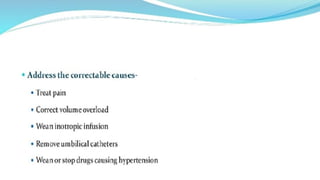
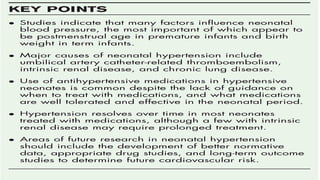
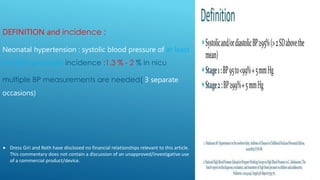
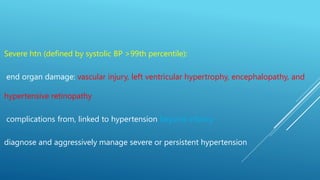
1) Neonatal hypertension is defined as a systolic blood pressure at or above the 95th percentile, with multiple measurements needed on separate occasions. The most common causes in newborns are issues related to umbilical catheters and renal problems.
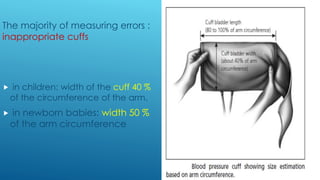
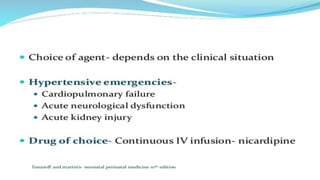
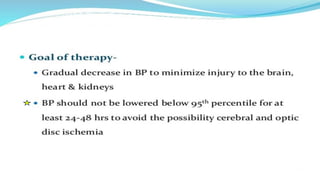
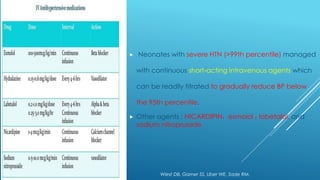
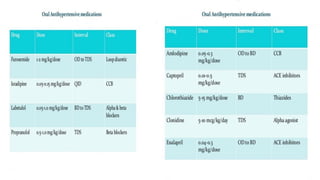
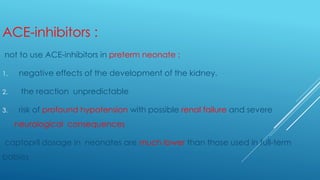
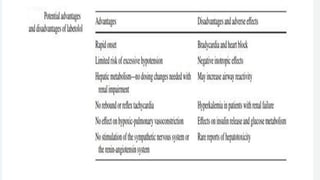
2) Proper measurement of blood pressure in infants requires an appropriately sized cuff. Treatment of severe hypertension in neonates involves intravenous antihypertensive drugs to gradually lower blood pressure below the 95th percentile.
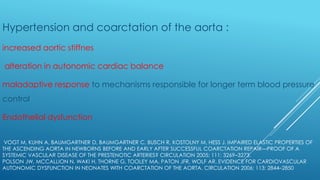
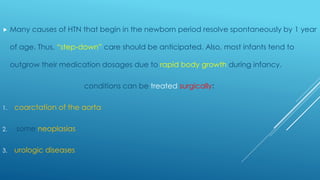
3) Common causes of hypertension change with age, from problems like renal artery stenosis in newborns to essential hypertension in adolescence. Many cases resolve by one year of age, but conditions like coarctation of the aorta may require
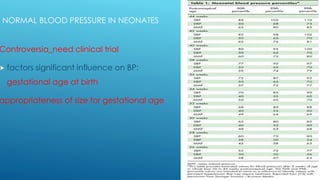

![ROUTINE EVALUATION OF BP IS NOT RECOMMENDED IN ALL
NEONATES (AAP)
routinely screening in the absence of symptoms does not usually apply
do not recommend routine screening, which should begin annually only at 3 years of
age.
recent AAP guidelines (Pediatrics. 2017;140[3]:e20171904
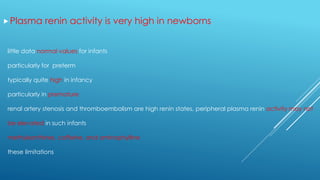
Hypertension was considerably more common in infants with:
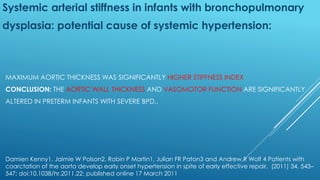
bronchopulmonary dysplasia
patent ductus arteriosus
and intraventricular hemorrhage
with indwelling umbilical arterial catheters
Antenatal steroids](https://image.slidesharecdn.com/dr-210205114622/85/HTN-in-heonates-and-infants-6-320.jpg)