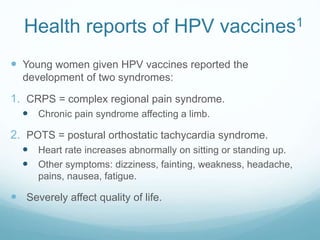
The document discusses two syndromes - complex regional pain syndrome (CRPS) and postural orthostatic tachycardia syndrome (POTS) - that some young women reported developing after receiving HPV vaccines. The European Medicines Agency reviewed the evidence and found no causal relationship between the HPV vaccines and the syndromes. They determined the rates of the syndromes were not significantly different between vaccinated groups and the general population. The conclusion was that CRPS and POTS are not linked to HPV vaccinations, and that all HPV vaccines remain safe and effective.