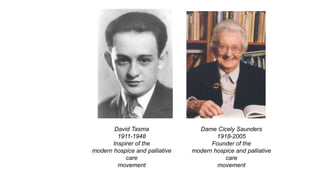
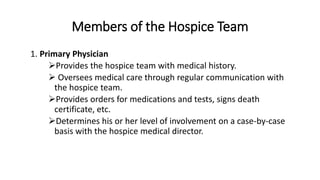
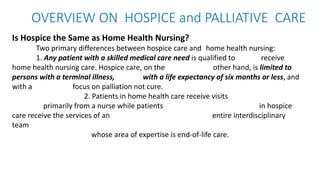
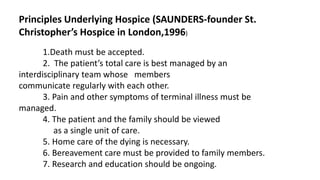
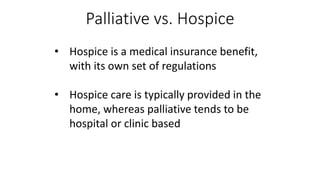
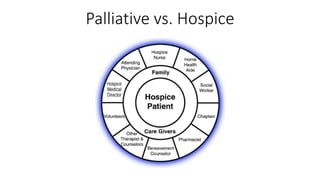
Hospice provides palliative care to patients with terminal illnesses through an interdisciplinary team approach. It focuses on comfort care and quality of life rather than cure. Dame Cicely Saunders founded the modern hospice movement in the 1960s based on her experience at St. Christopher's Hospice in London. Hospice care can be provided in the home, nursing home, hospital, or independent hospice facility. The hospice interdisciplinary team includes doctors, nurses, social workers, chaplains, home health aides, and volunteers who provide holistic physical, emotional and spiritual support to patients and their families.