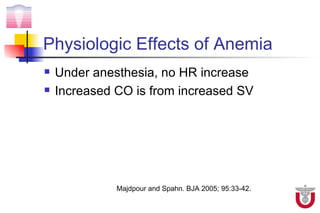
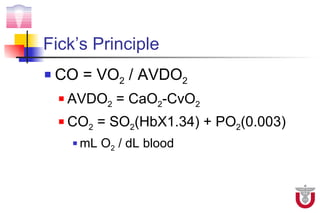
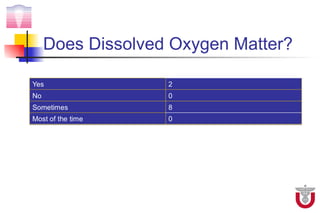
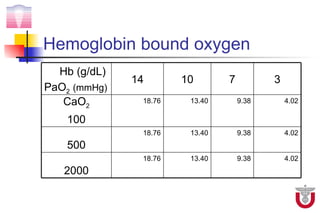
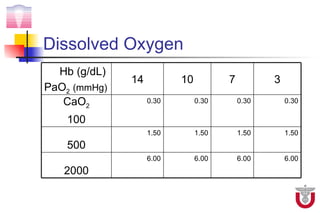
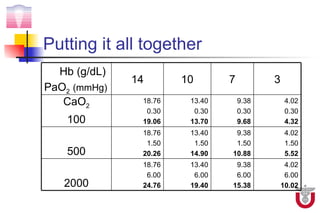
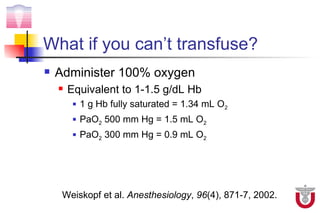
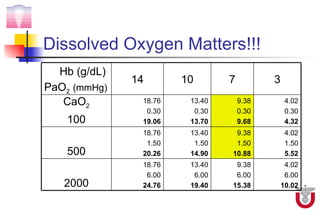
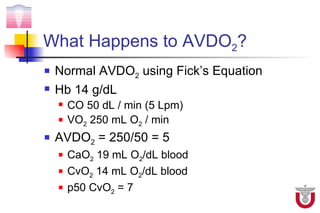
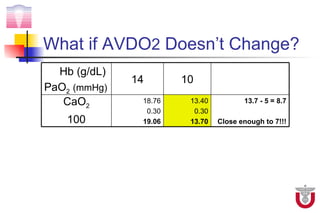
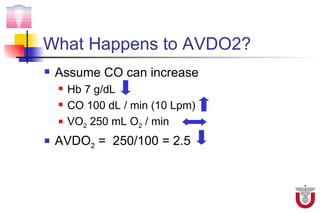
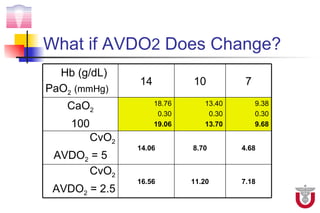
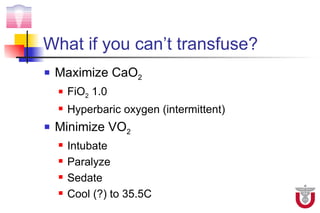
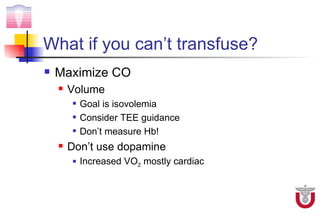
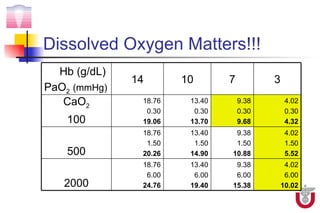
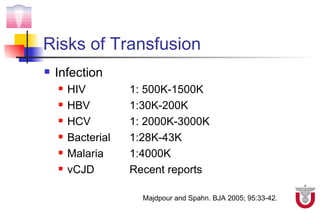
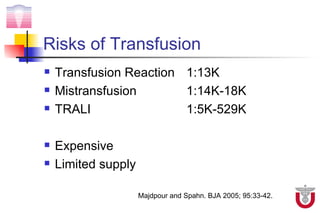
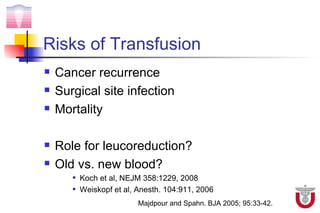
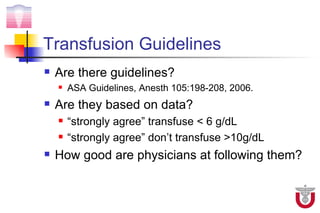
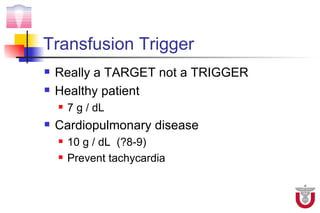
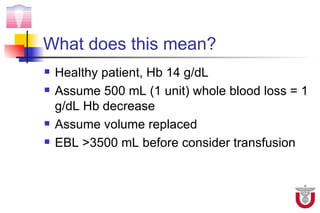
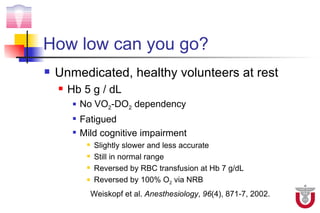
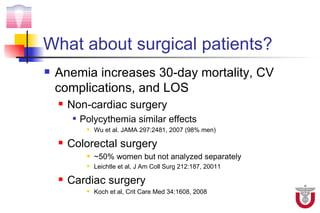
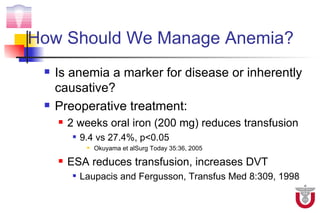
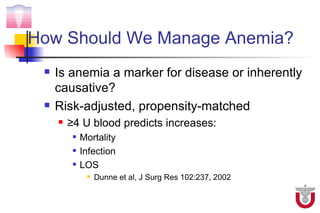
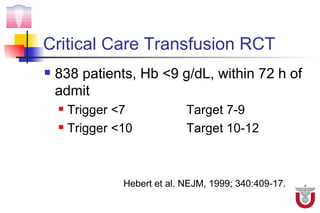
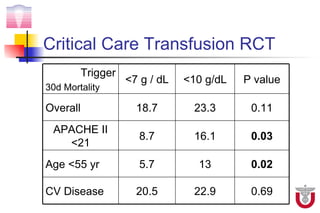
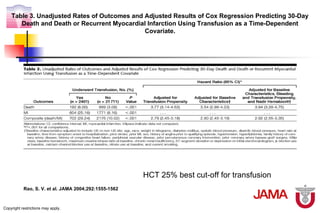
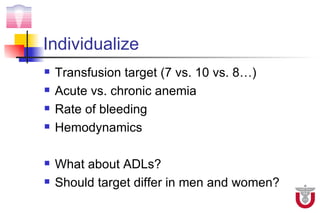
The document discusses transfusion triggers and when to transfuse red blood cells. It summarizes that the decision to transfuse should be based on individual patient factors like comorbidities, hemodynamics, and rate of bleeding rather than a single hemoglobin threshold. While guidelines recommend transfusion at Hb <7 or <10, clinical trials found higher transfusion triggers were not associated with better outcomes and increased risks. Physiologic compensation for anemia through increased cardiac output and dissolved oxygen delivery means lower hemoglobin levels may be tolerated without transfusion in some cases.