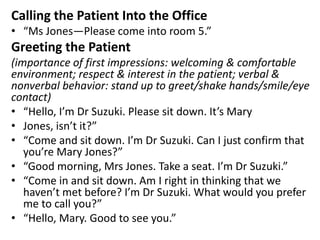
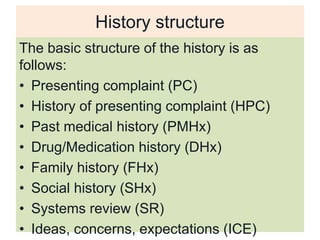
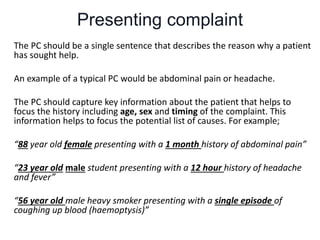
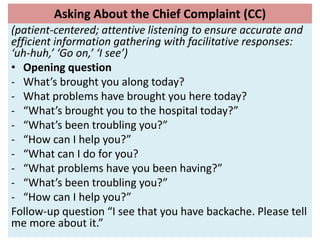
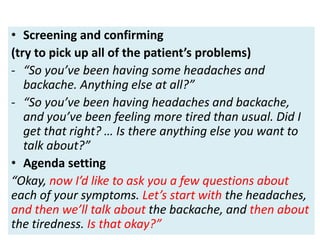
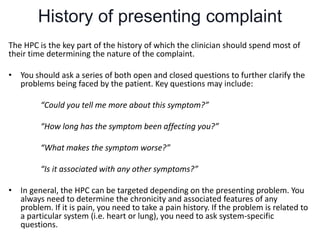
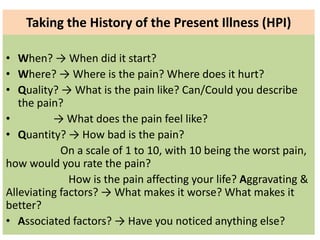
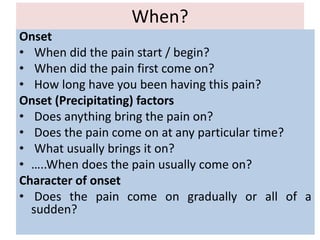
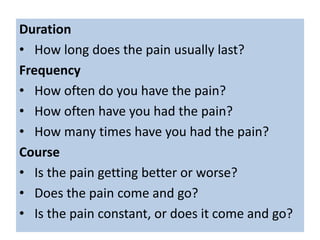
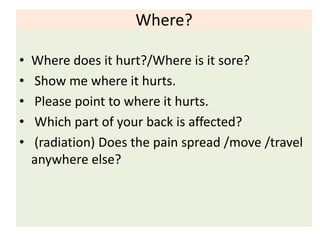
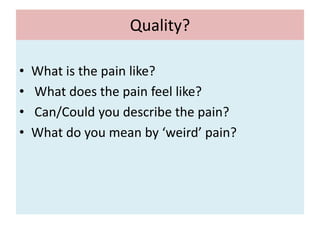
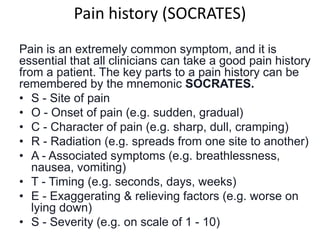
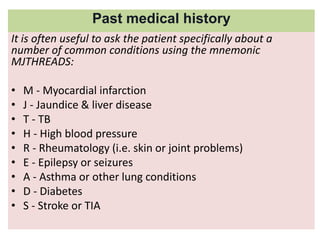
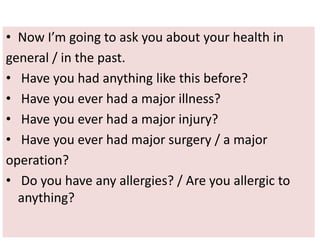
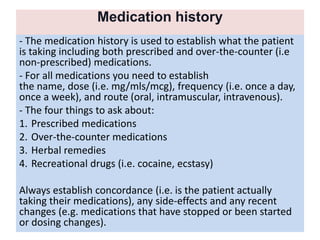
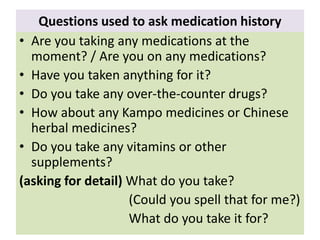
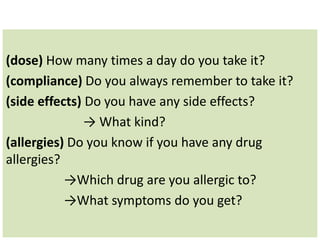
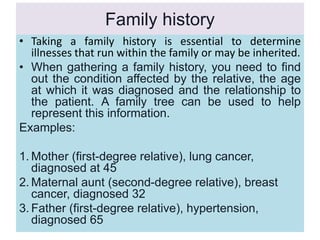
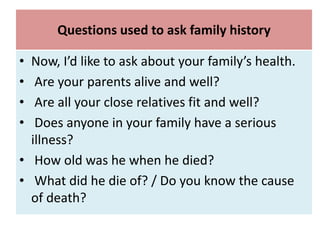
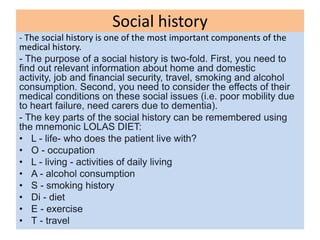
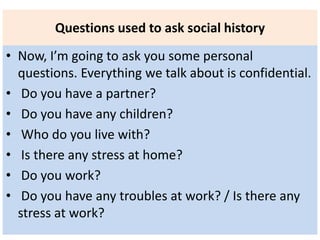
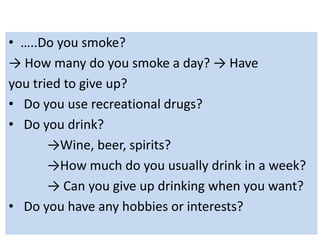
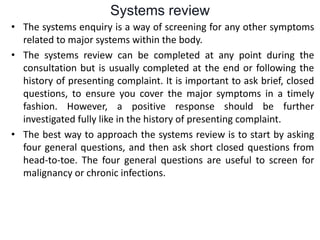
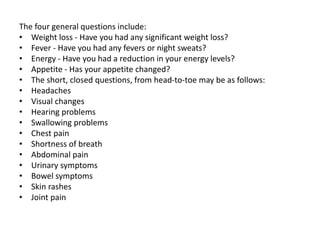
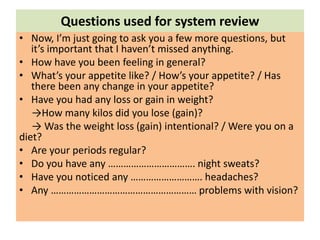
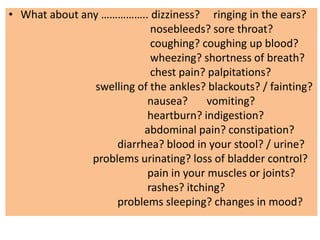
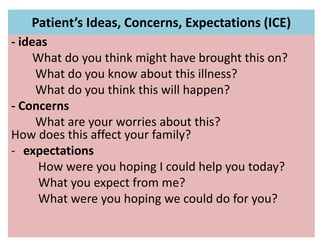
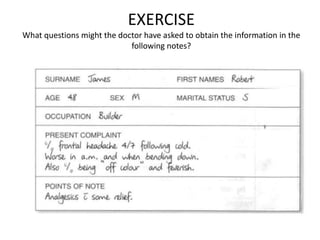
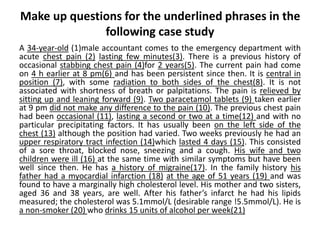
The document outlines the process of taking a medical history from a patient, detailing aspects such as greetings, the structure of the history, and key components like presenting complaints, past medical history, and social history. It emphasizes the importance of patient-centered questioning techniques to gather comprehensive information while building rapport. Various mnemonics like 'SOCRATES' and 'MJTHREADS' are introduced to aid in the efficient collection of relevant medical data.