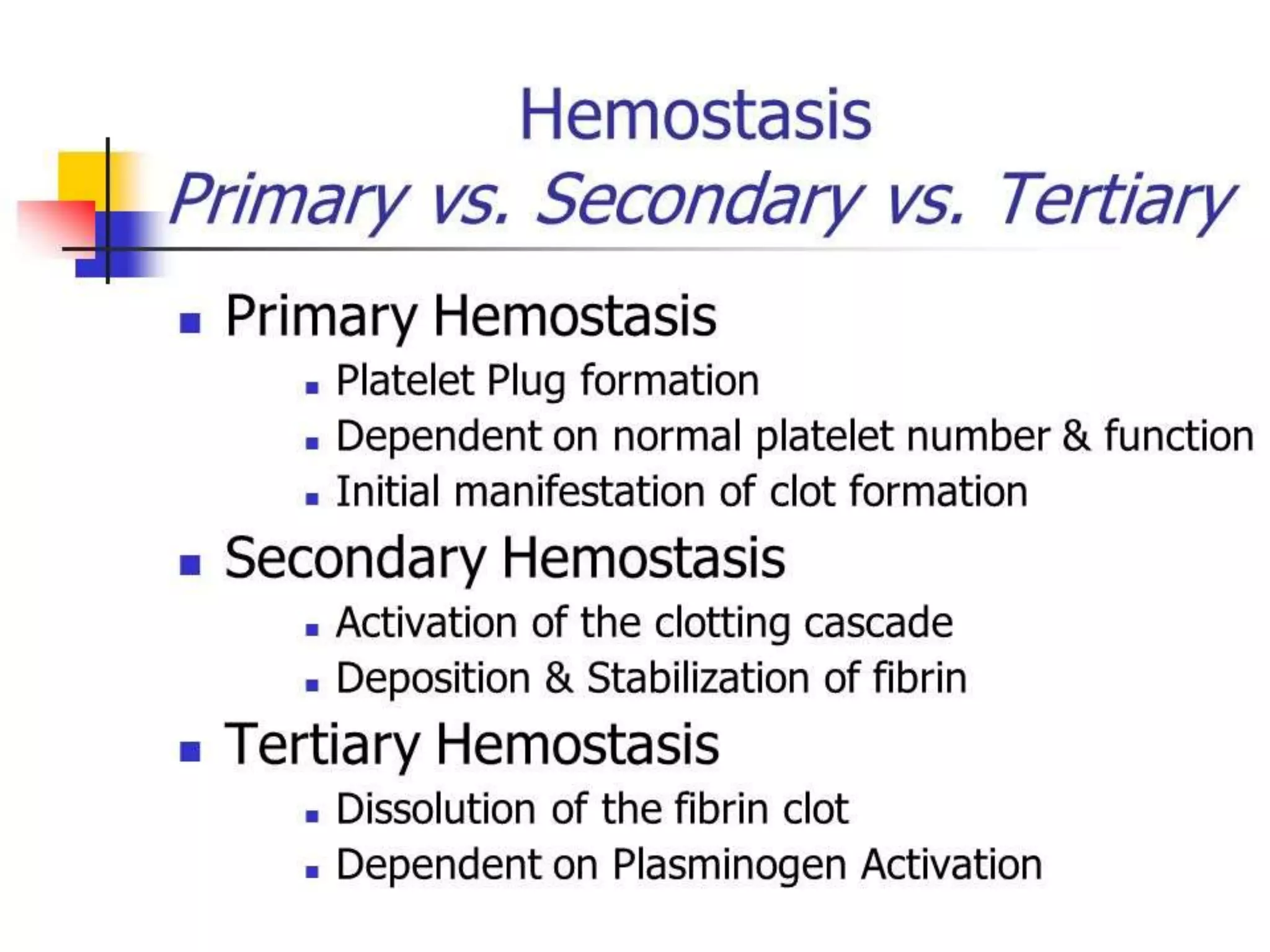
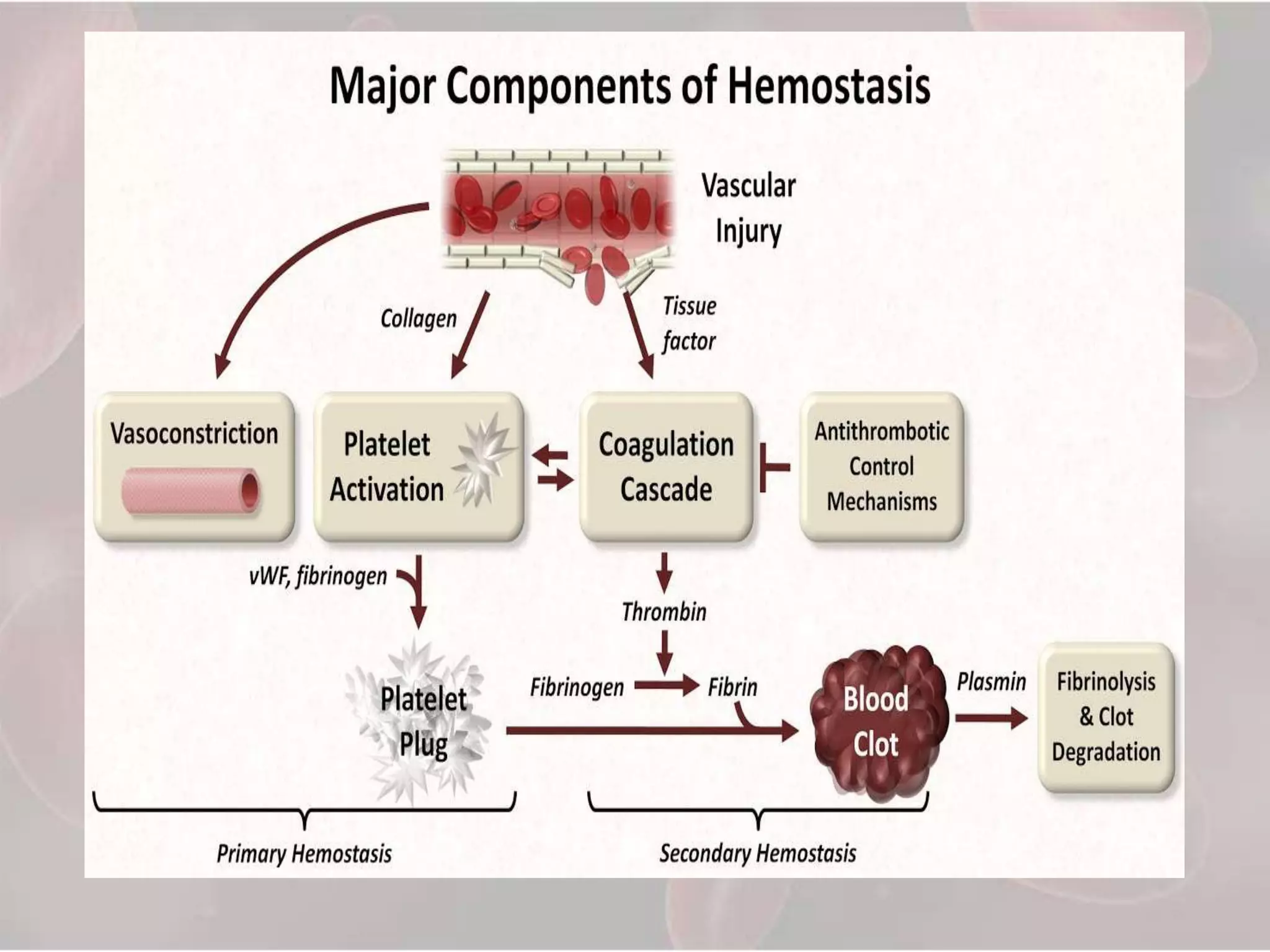
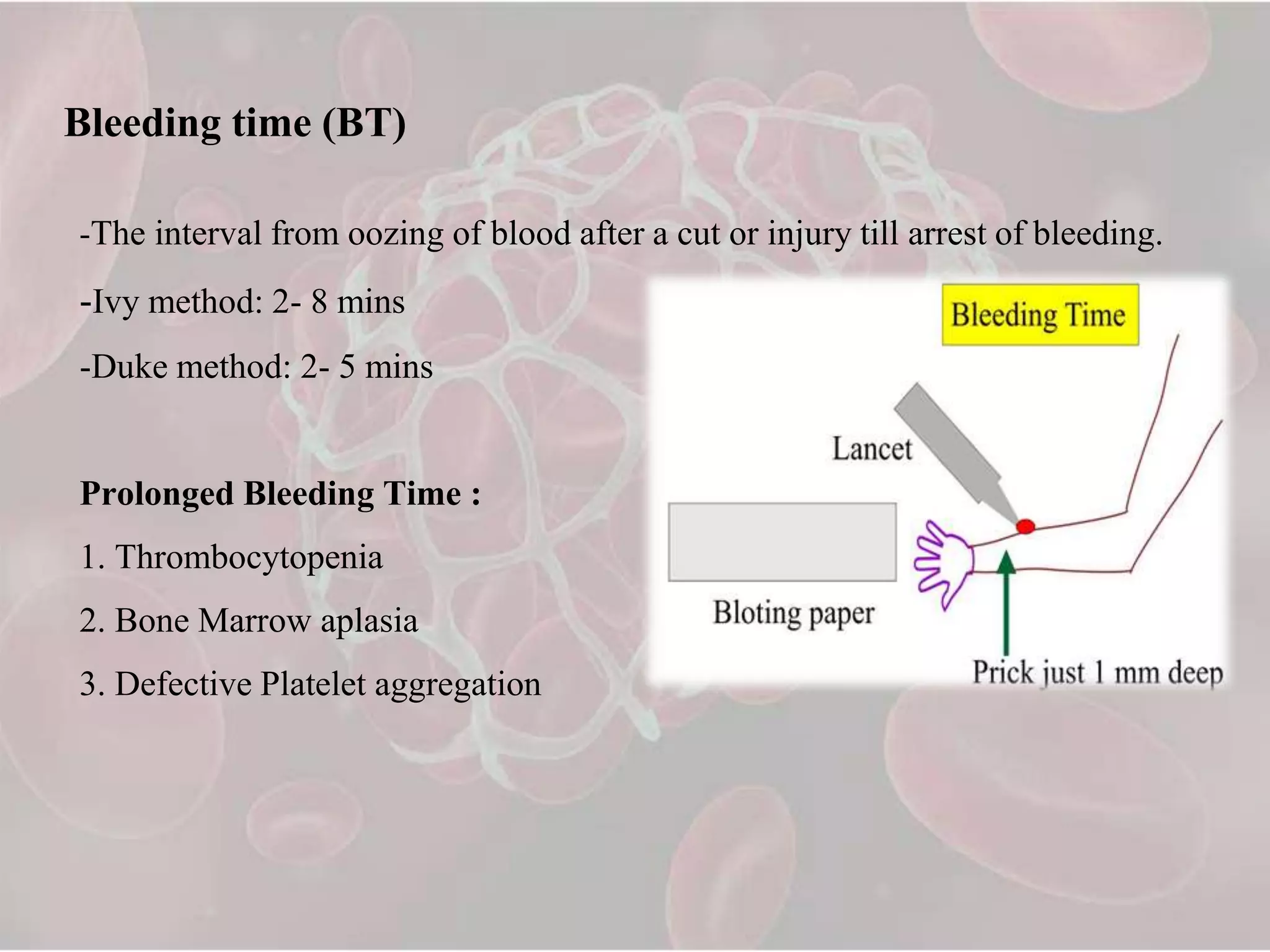
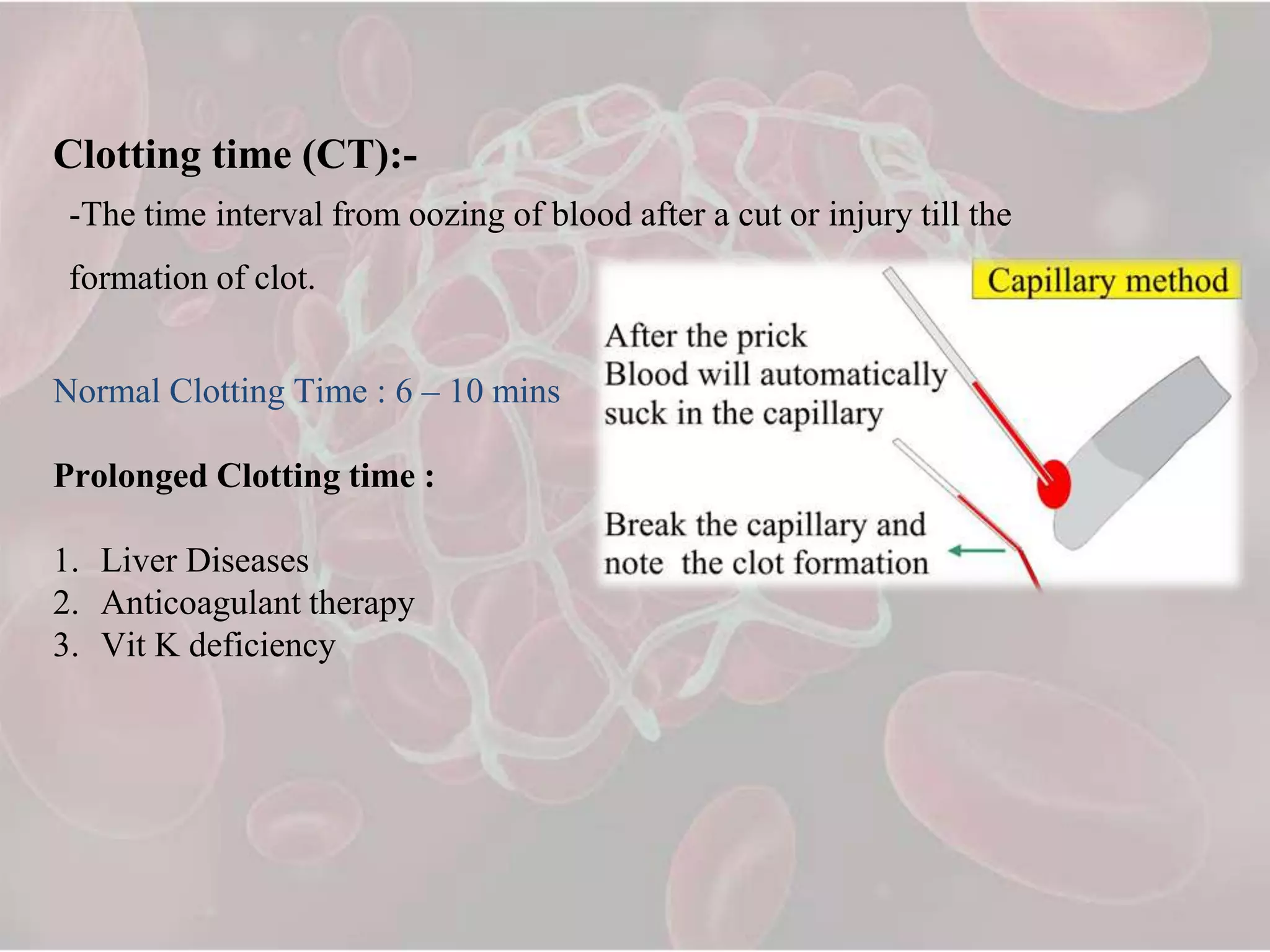
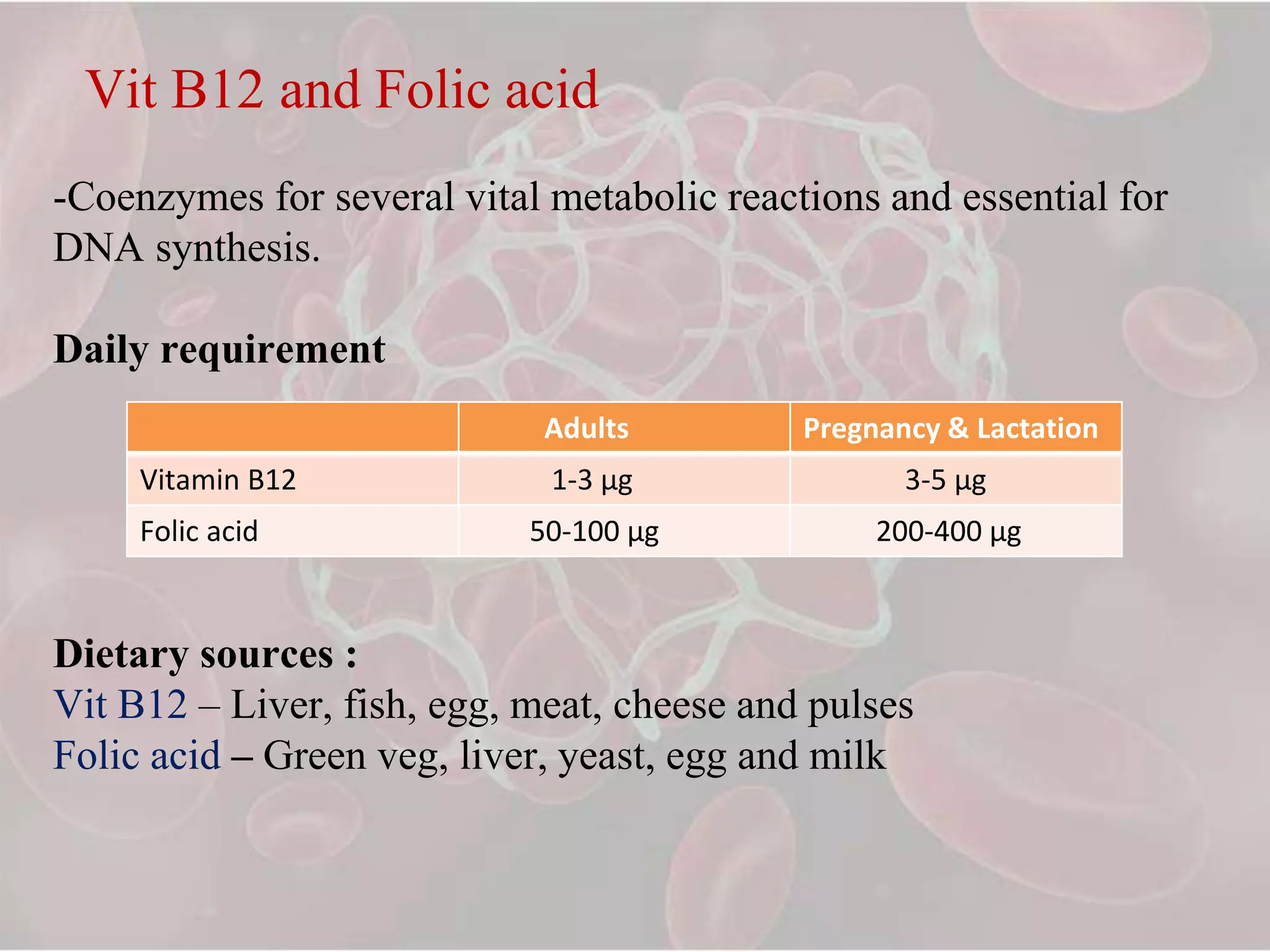
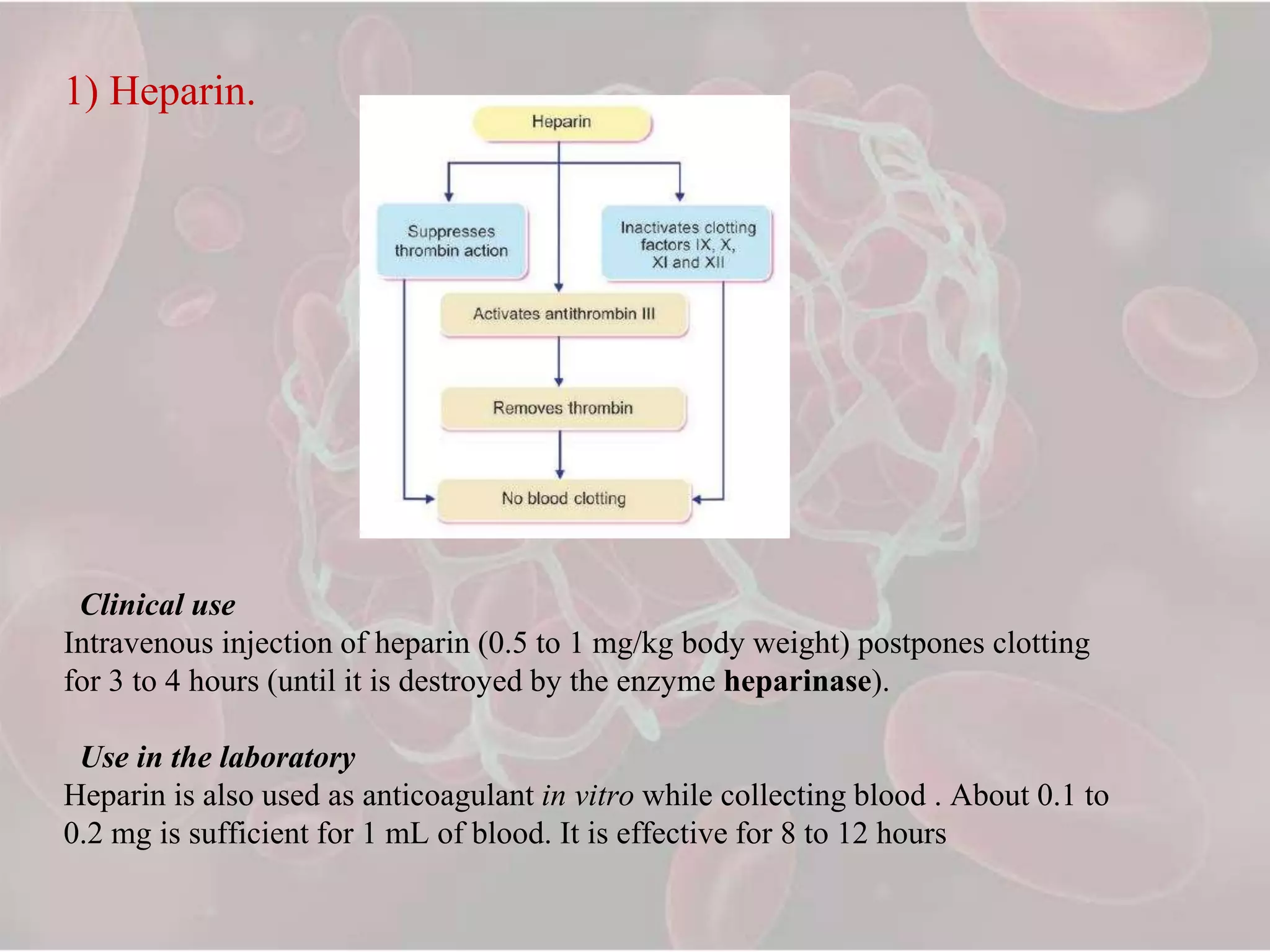
The document provides an overview of hemostasis, detailing the physiological mechanisms involved, including vascular constriction, platelet plug formation, and blood coagulation. It discusses blood coagulation tests and their significance, as well as the roles of hematinics, coagulants, and anticoagulants in maintaining hemostasis and treating bleeding disorders. Additionally, it covers various techniques and substances used to promote coagulation and manage bleeding in clinical settings.