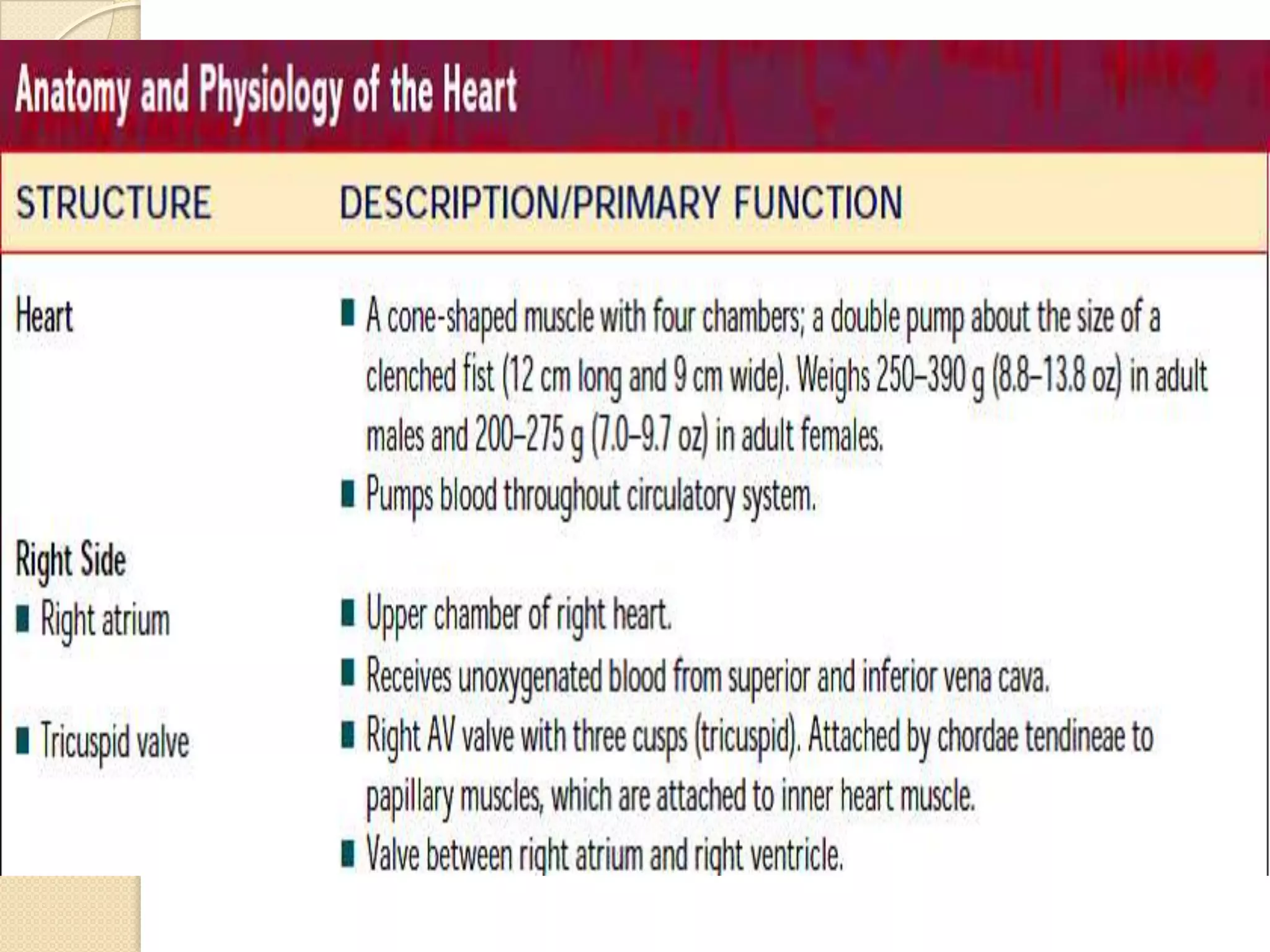
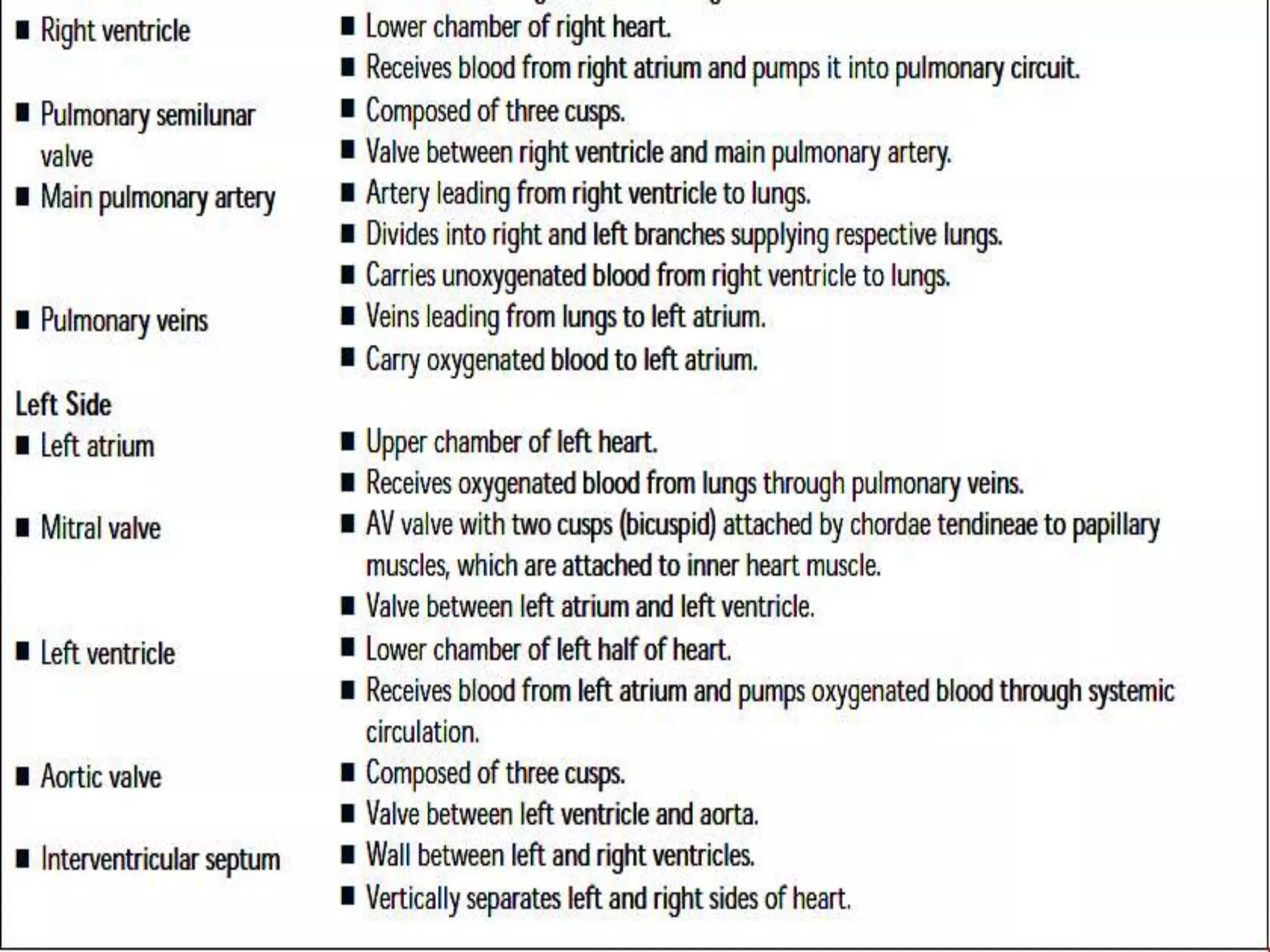
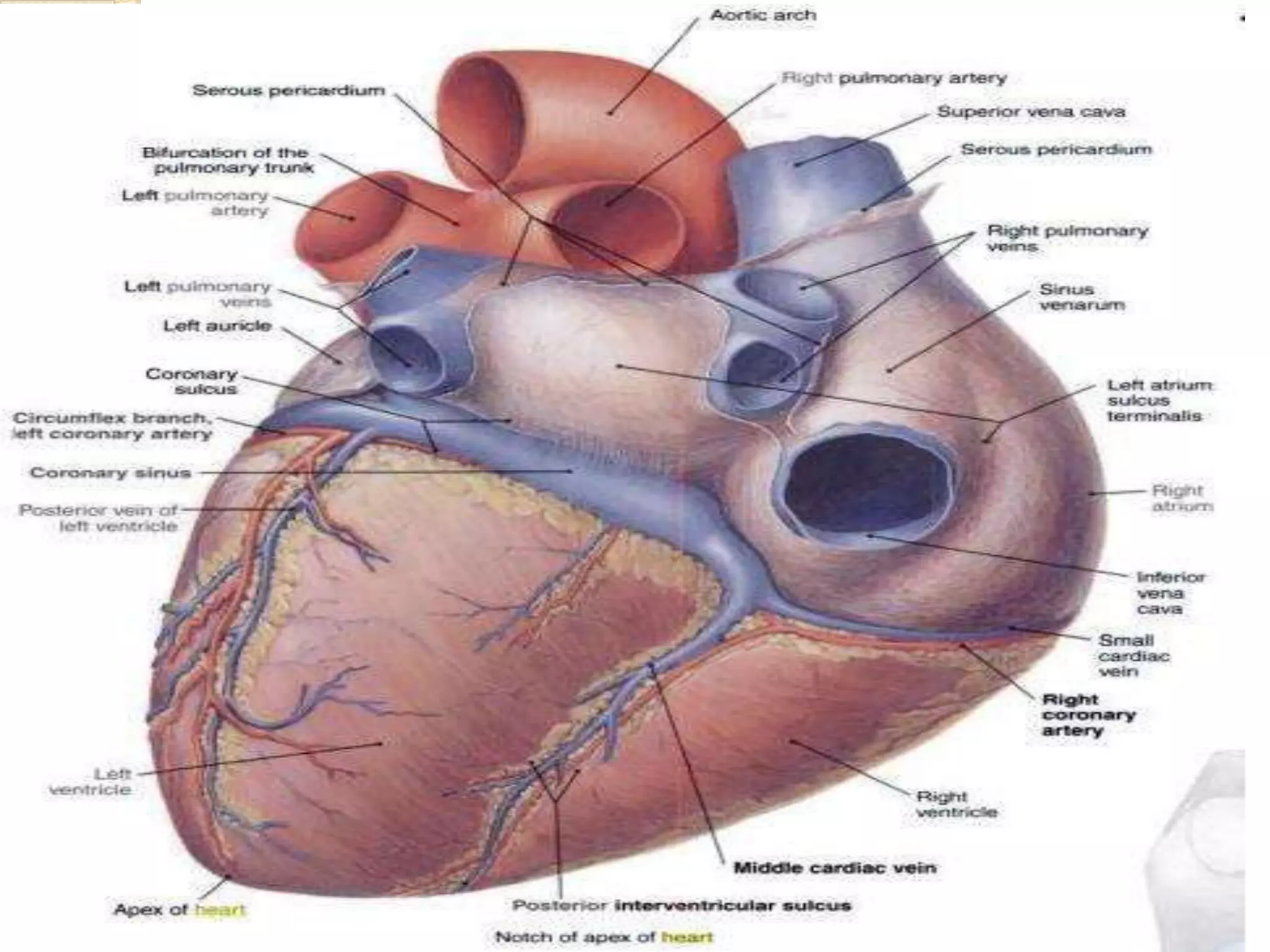
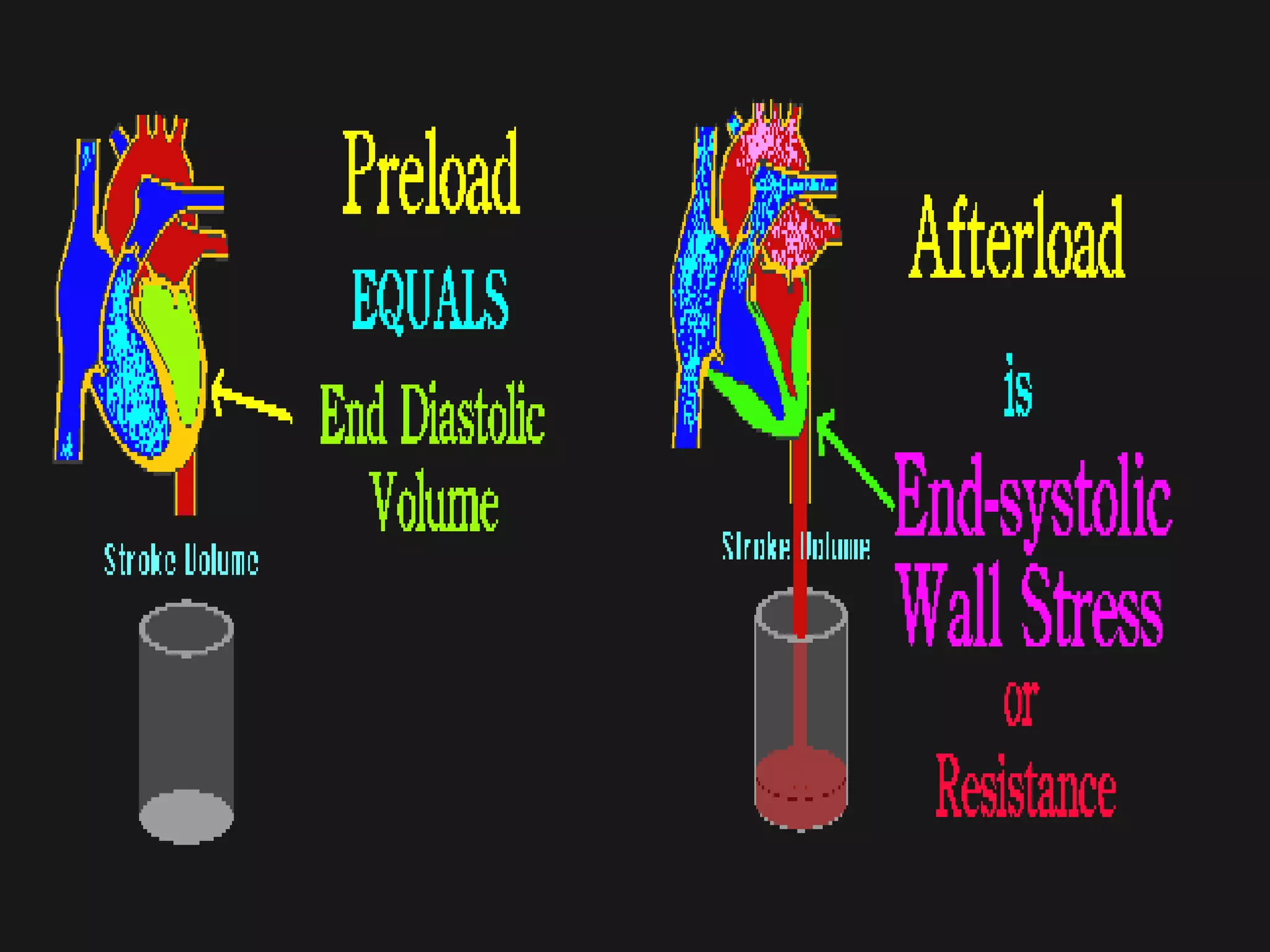
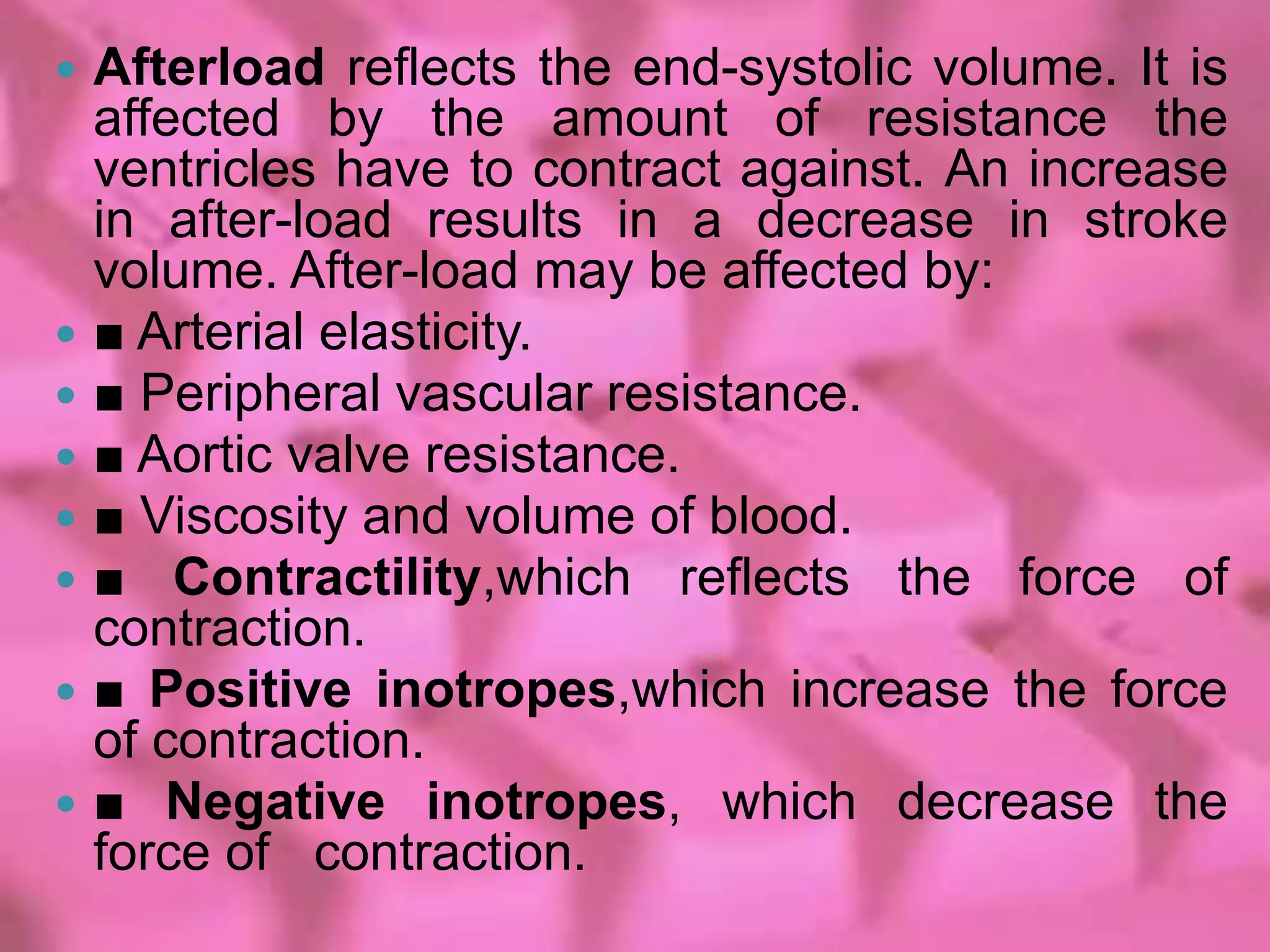
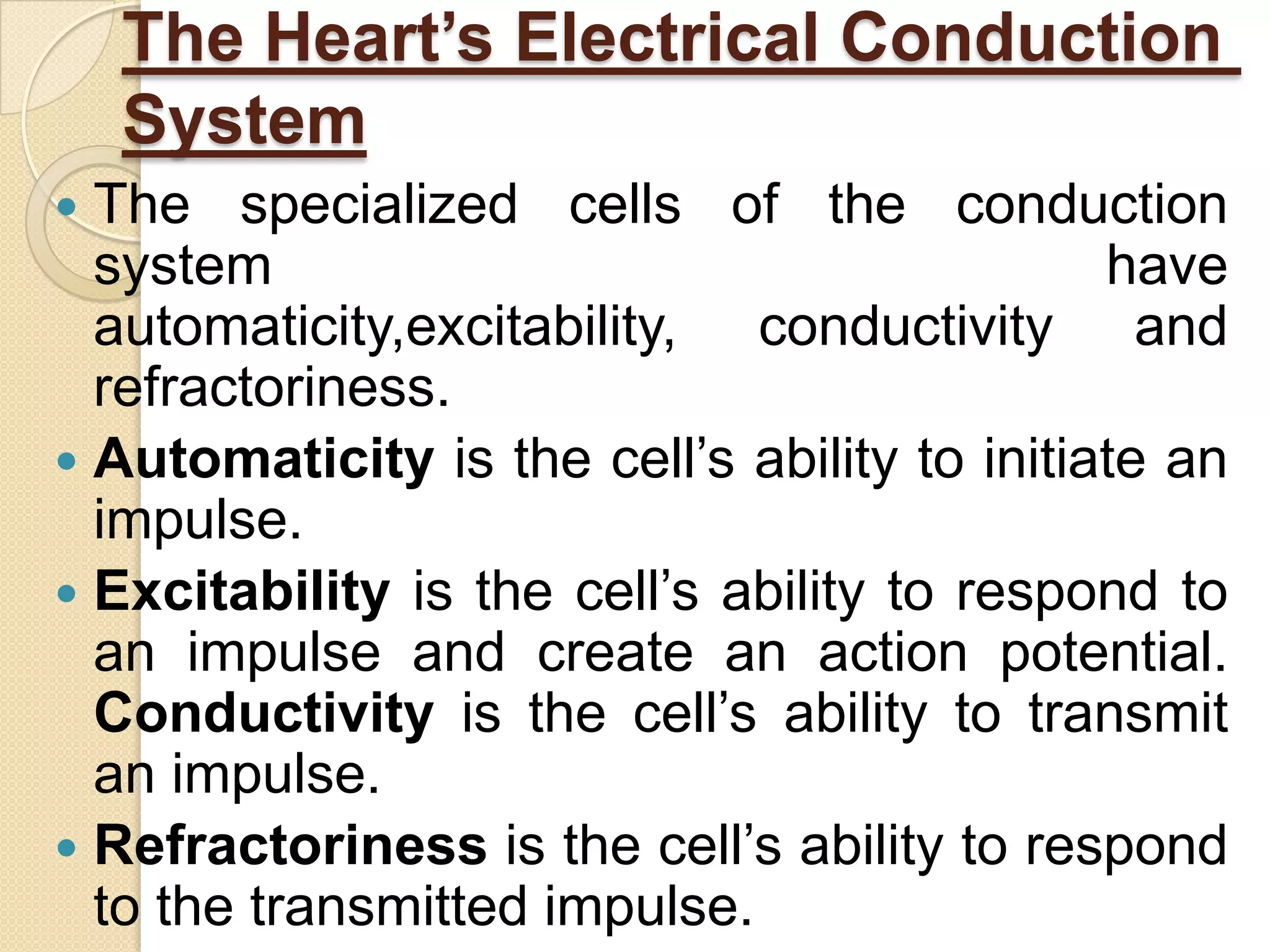
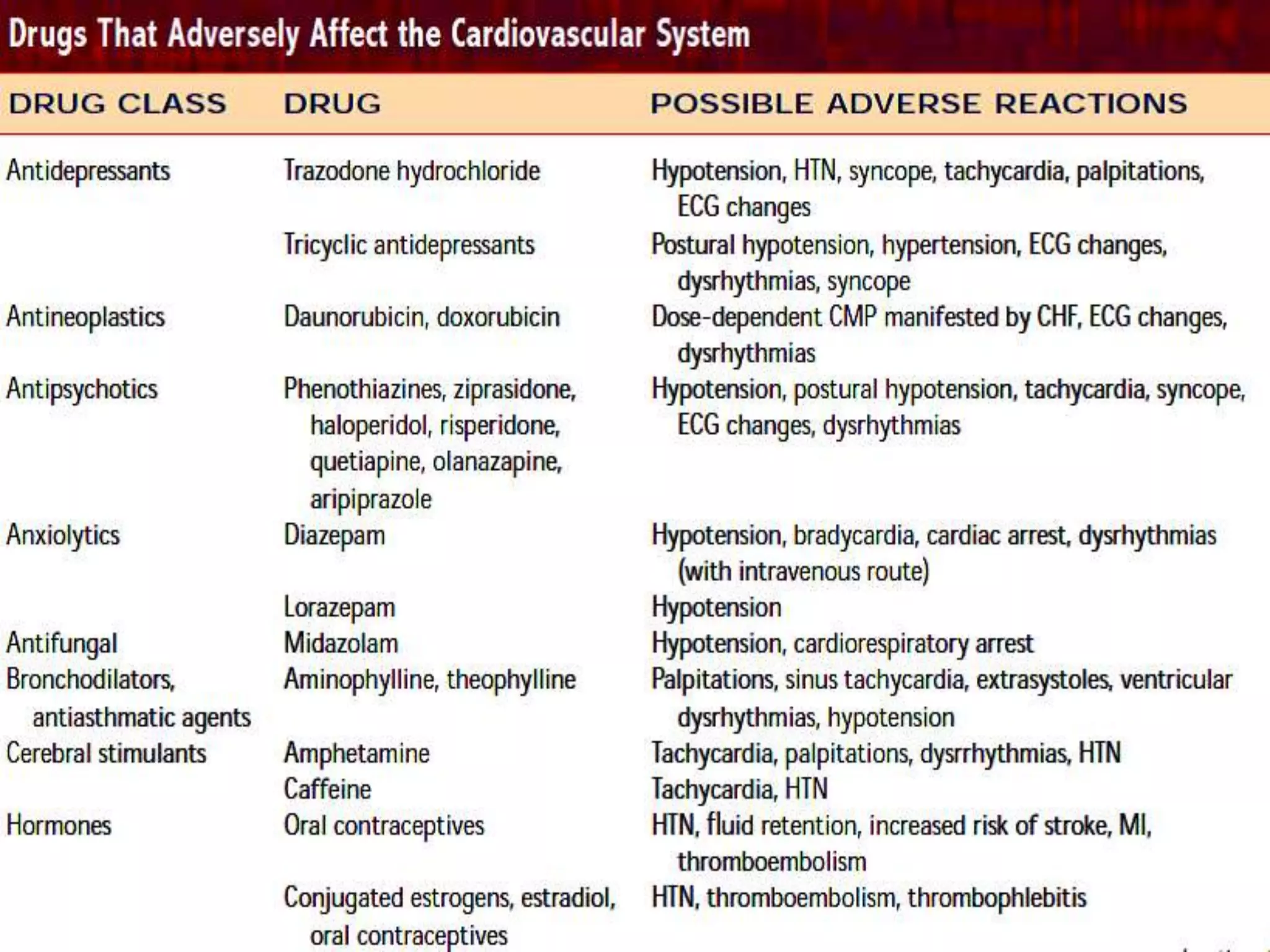
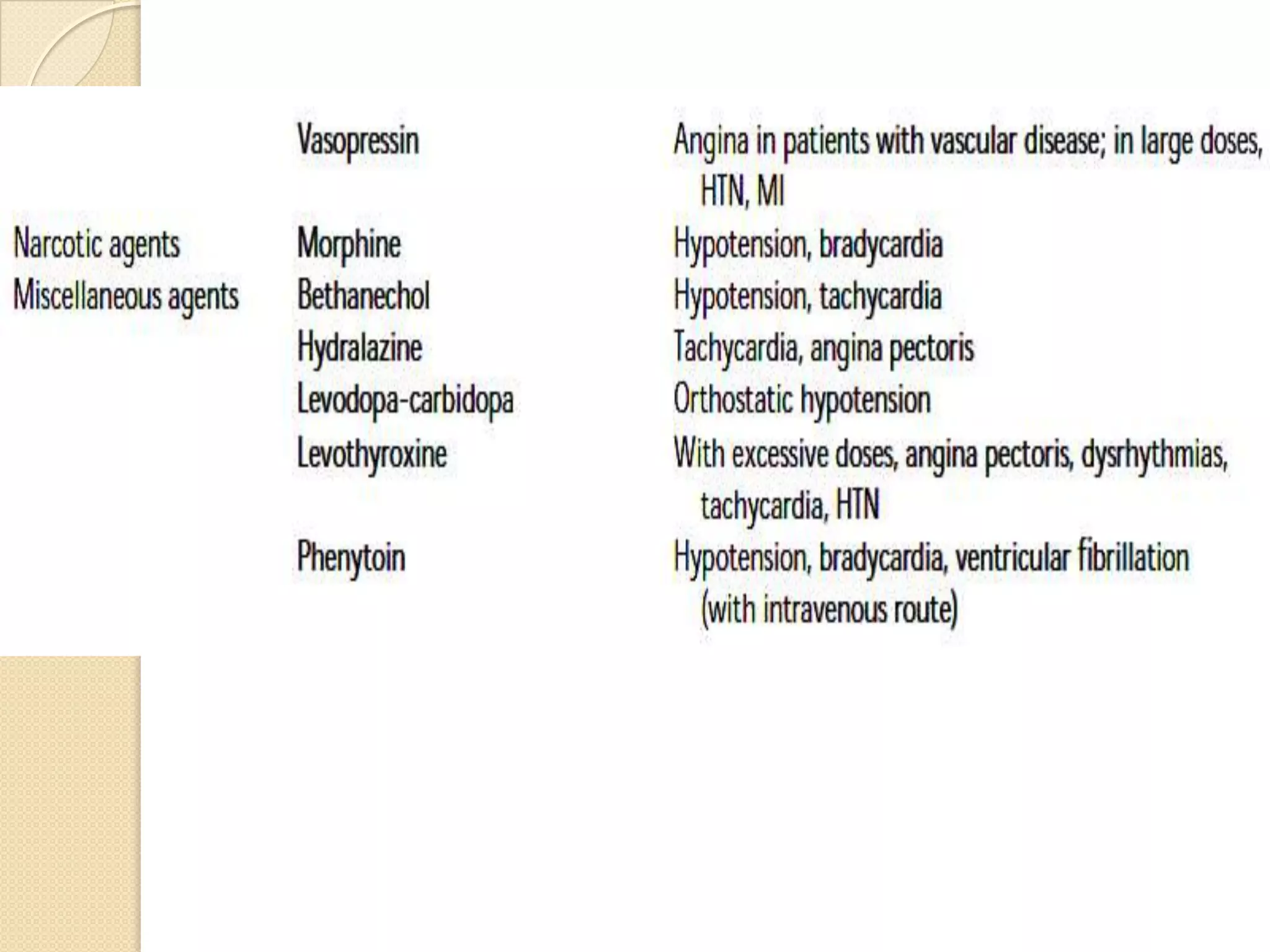
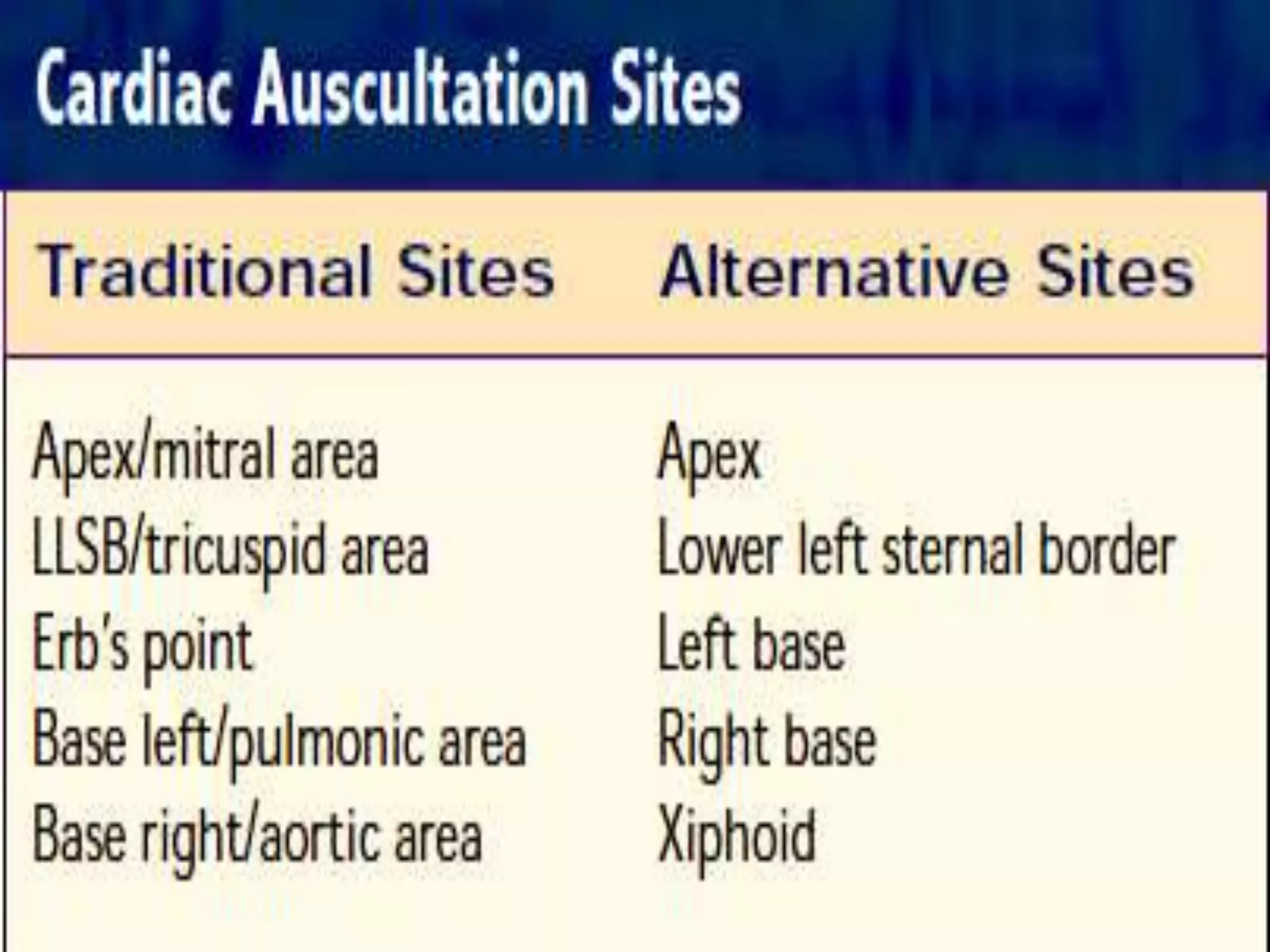
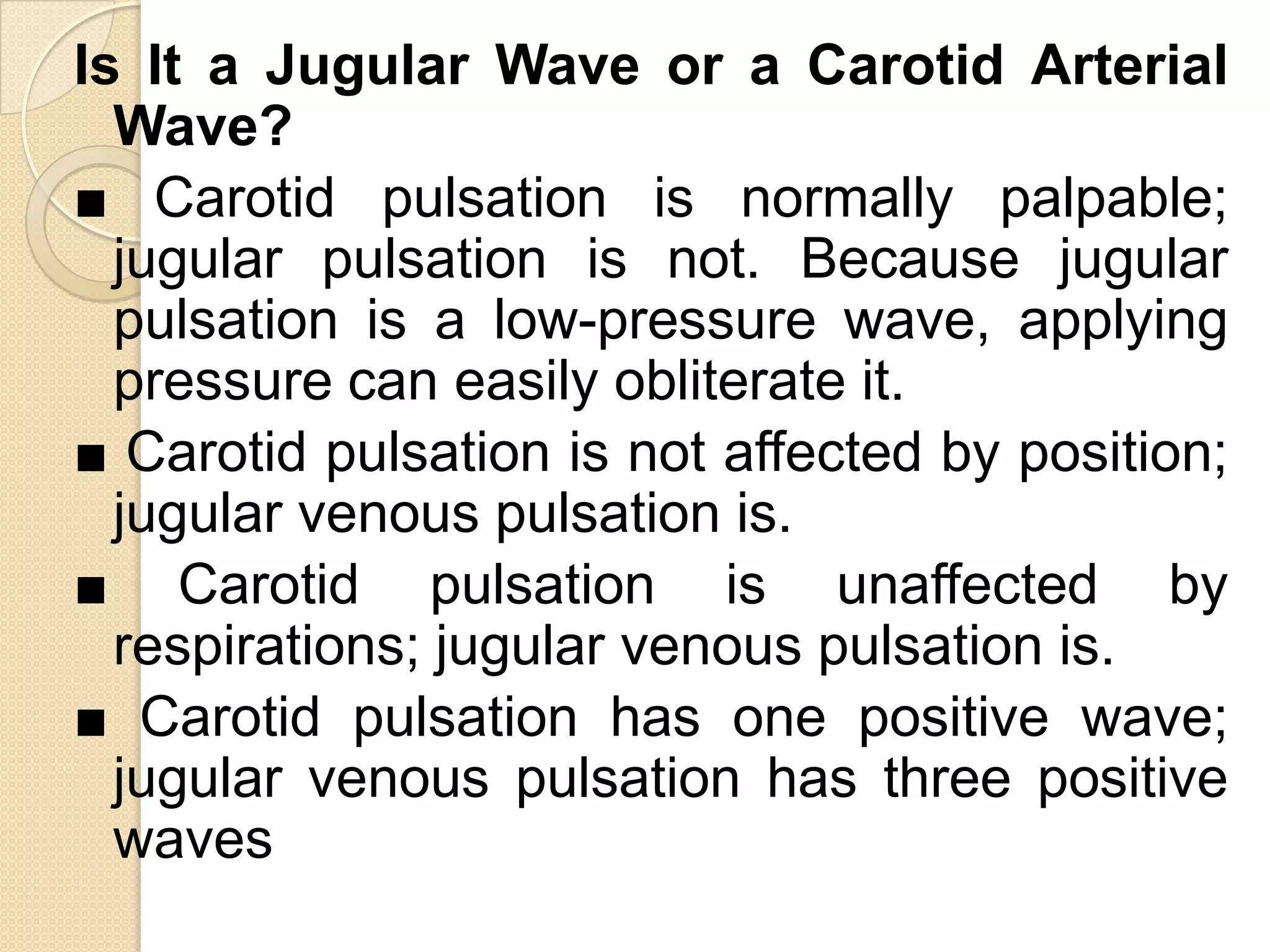
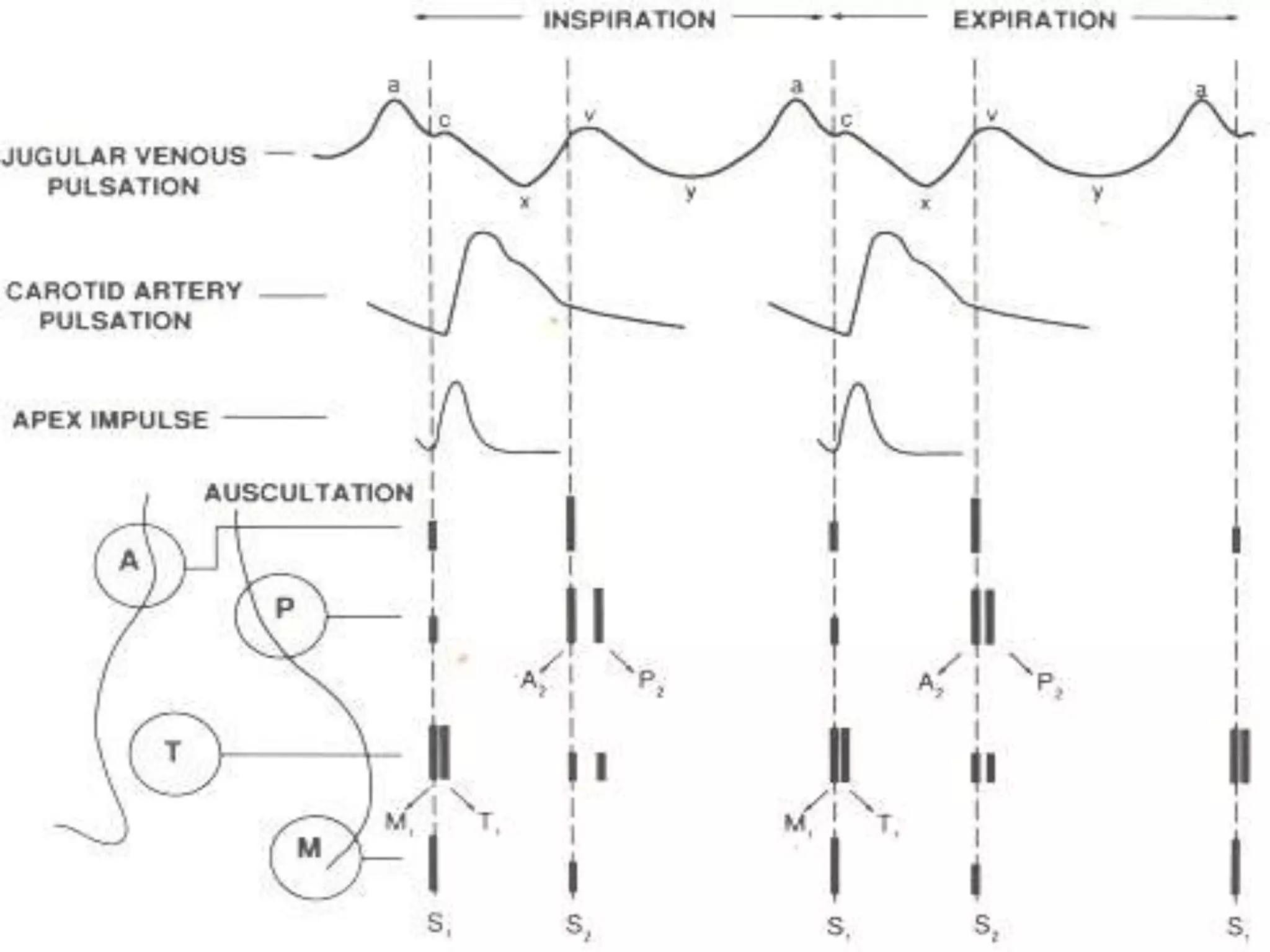
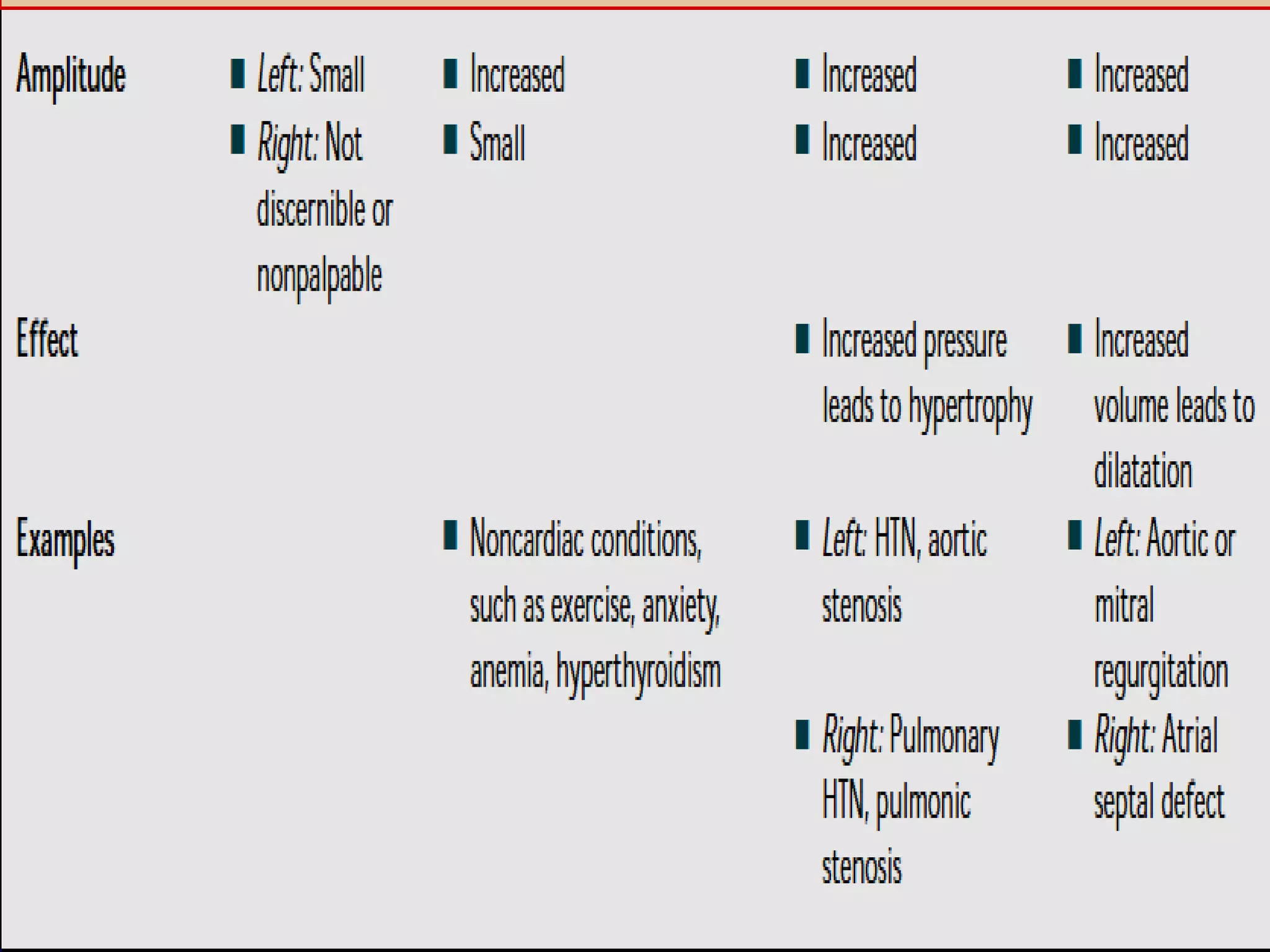
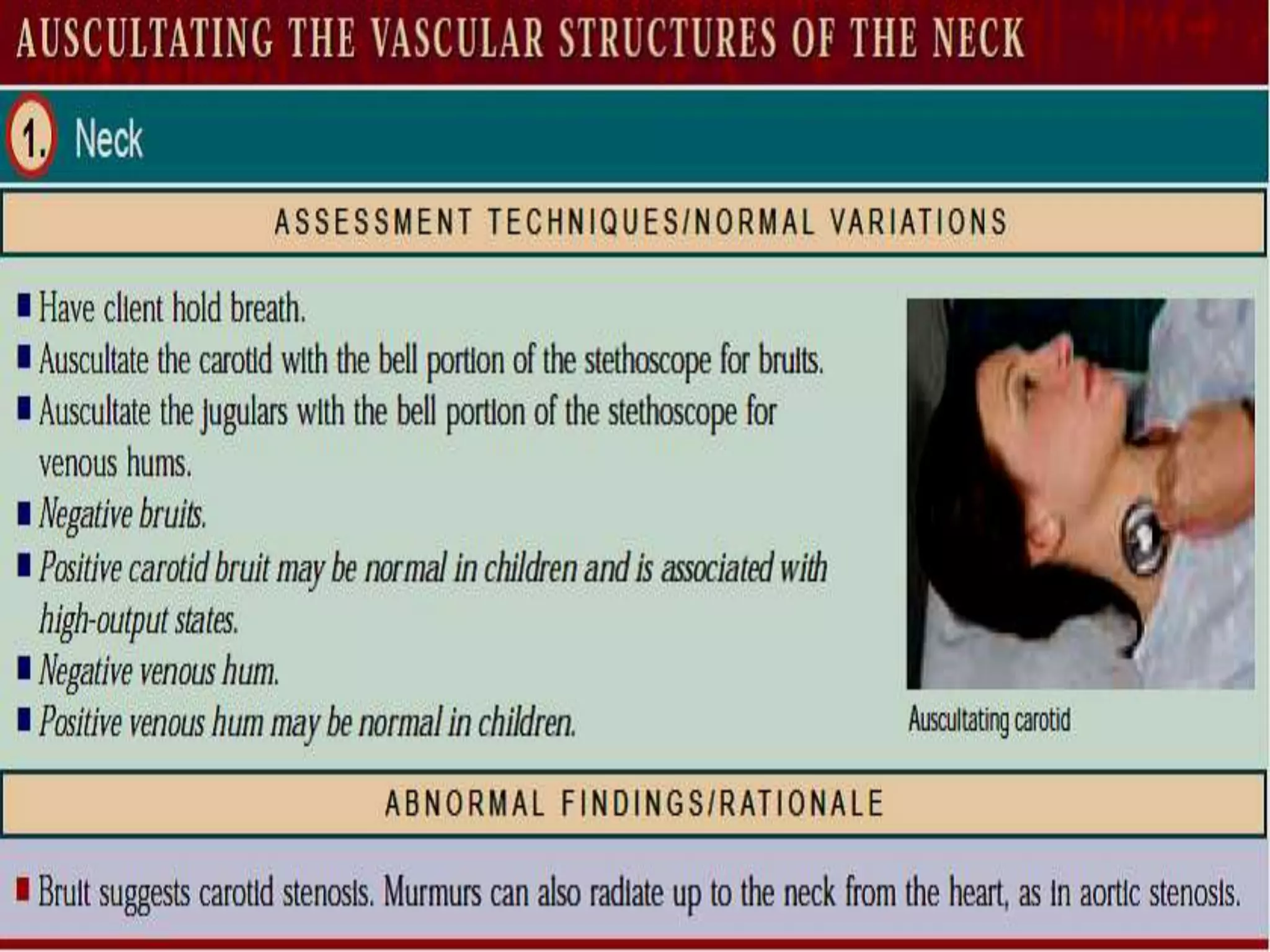
This document describes the layers of the heart and the cardiovascular system, including the circulatory, electrical conduction, and valvular components. It explains the cardiac cycle and how factors like preload and afterload impact stroke volume. Key anatomical structures are defined, such as the sinoatrial node, atrioventricular node, and bundle of His. Normal heart sounds, murmurs, and pulsations are characterized. Interactions between the cardiovascular system and other body systems are also outlined.