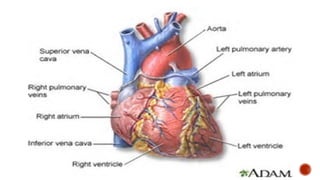
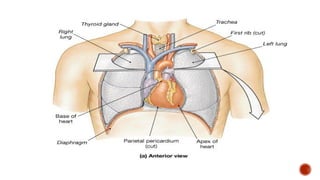
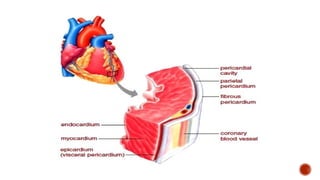
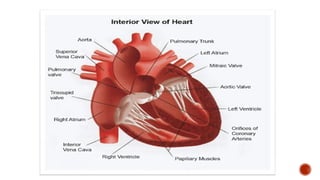
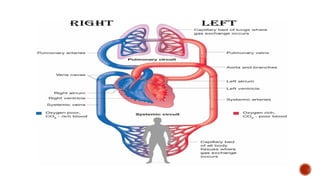
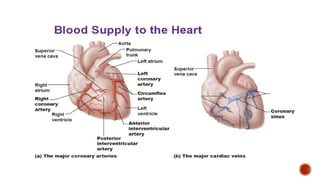
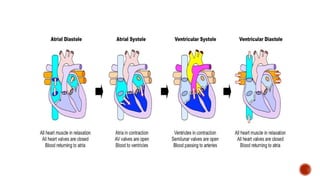
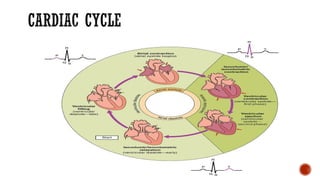
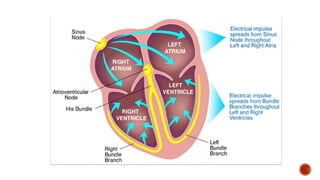
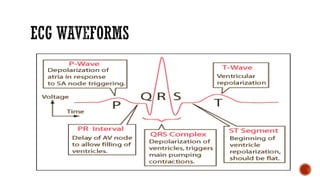
The document provides a comprehensive overview of the cardiovascular system, including the major structures and functions of the heart, blood circulation, and the cardiac cycle. Key components such as the heart's anatomy, the conduction system, and the physiological processes during heartbeats are detailed, alongside explanations of cardiac output and ejection fraction. Additionally, it discusses systemic, pulmonary, and coronary circulation and the regulation of blood flow through various heart structures.