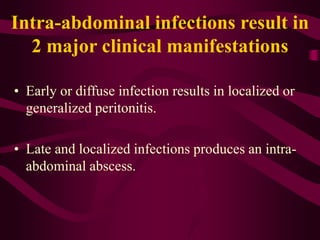
Peritonitis is an infection or inflammation of the peritoneum, the membrane lining the abdominal cavity. There are two major types - primary peritonitis caused by spread of infection through the bloodstream and secondary peritonitis caused by a rupture or leak in the gastrointestinal or biliary tract. Symptoms include abdominal pain and tenderness, fever, nausea, and difficulty breathing. Treatment involves antibiotics, surgery to address the infection source, pain medication, and IV fluids. With treatment, prognosis depends on the underlying cause but untreated peritonitis is often fatal.